George J Tolis
MD PhD CSPQ FRCP(Can)
Director
Division of Endocrinology and Metabolism
Hippokrateion Hospital
Vice President Central Health Council
Ministry of Health Athens, Greece
Anthi A Protonotariou
MD
Research Assistant Endocrinologist
Division of Endocrinology and Metabolism
Hippokrateion Hospital
Athens, Greece
Gonadal steroids are of primary importance in male physiology throughout life. In utero, testosterone and its potent metabolite, dihydrotestosterone (DHT), are necessary for normal differentiation of the genital ducts and external genitalia along male lines. During puberty a series of androgen-mediated physical, metabolic and behavioural/ psychological changes take place, which lead to the phenotype of the mature male and provide reproductive capacity to the individual. After pubertal development has been completed, gonadal steroids are necessary to maintain virilisation, sexual function and normal spermatogenesis/ fertility, as well as musculoskeletal integrity and strength.
Testosterone replacement therapy (TRT) is indicated primarily in male hypogonadism associated with decreased testosterone production and related to primary testicular failure (hypergonadotropic hypogonadism), or hypothalamic-pituitary disease (hypogonadotropic hypogonadism). Irrespective of the aetiology of hypogonadism, clinical manifestations of androgen deficiency depend primarily on the age of the patient at the time of onset of the disorder.
Hypogonadism: clinical presentation, evaluation
Impaired testosterone secretion, metabolism or action during fetal life is associated with incomplete masculinisation of the male fetus (male pseudohermaphroditism). Prepubertal androgen deficiency results in absent or incomplete pubertal development: a male with poor secondary sex characteristics and eunuchoid skeletal proportions (long arms and legs). In contrast, hypogonadism that develops postpubertally leads to slowly evolving subtle clinical symptoms and signs, which are often ignored by the physician or denied by the patient: loss of libido, impotence, low energy and mood disturbances, slowing of body hair growth with a decrease in the frequency of shaving, progressive decrease in muscle mass, increased risk of osteoporosis/fractures and infertility.
Initial laboratory evaluation should include measurements of plasma morning testosterone levels in conjunction with sex hormone-binding globulin (SHBG) levels, basal plasma follicle-stimulating hormone (FSH) and luteinising hormone (LH) levels, to distinguish between hypergonadotropic and hypogonadotropic states, and semen analysis. Prolactin (PRL) levels should be measured in all patients with hypogonadotropic hypogonadism. Specialised hormonal dynamic testing, genetic studies and imaging procedures are helpful in the differential diagnosis of hypogonadism and should be performed if they are indicated by baseline diagnostic testing.
Testosterone replacement therapy
As soon as the diagnosis of androgen deficiency has been established, adequate hormone replacement therapy should be instituted. The goals of testosterone replacement therapy in hypogonadal patients are to:
- Promote/maintain virilisation.
- Restore sexual function, libido and wellbeing.
- Optimise bone density and prevent osteoporosis.
In patients with hypogonadotropic hypogonadism, genetic or acquired, long-term exogenous gonadotropin therapy or pulsatile subcutaneous gonadotrophin-releasing hormone (GnRH) administration through a portable pump (if only pituitary gonadotrophs are anatomically and functionally intact) will initiate pubertal development, maintain virilisation and sexual function, and initiate/maintain spermatogenesis. However, due to the expense and inconvenience of this type of therapy, it is usually reserved for patients with hypogonadotropic hypogonadism who desire fertility, in order to induce spermatogenesis.
The treatments listed in Table 1 are nontoxic. A diurnal rhythm of plasma testosterone, mimicking the normal circadian variation, is achieved with transdermal preparations. Dose selection and adjustment should be individualised. Ideally, testosterone therapy should provide physiological range serum testosterone, DHT and oestradiol levels.
[[HPE07_table1_80]]
Patients with hypogonadism of prepubertal onset should be gradually virilised: testosterone therapy is initiated with low doses (50mg of testosterone-ester every three to four weeks), which is gradually increased to full replacement dose, as tolerated, within one year. If high doses are administered from the start, dose-related adverse effects, such as frequent erections/priapism, acne and behavioural disturbances may be seen.
Contraindications
The presence of prostatic carcinoma is an absolute contraindication for testosterone administration. Obstructive benign prostate hyperplasia, male breast cancer, as well as polycythaemia and sleep apnoea/COPD in overweight or heavy smokers are relative contraindications to the use of androgen therapy.
Side-effects
- Exacerbation of prostatic disease.
- Polycythaemia.
- Sleep apnoea.
- Water and sodium retention.
- Gynaecomastia.
- Hepatotoxicity (rare).
- Suppression of spermatogenesis (supraphysiological doses of testosterone).
Monitoring of patients during TRT
Periodic follow-up is needed. During the first year of therapy the clinical response and the eventual development of side-effects should be monitored at three- to four-month intervals. Testosterone levels should be monitored periodically to ensure the appropriate range is maintained. Examination of the prostate should be done routinely. Prostate-specific antigen (PSA) levels should be determined at least annually in older men, and the haematocrit every six months for the first 18 months of therapy and then yearly if it remains stable. An initial lipid profile should be recorded, and a follow-up profile should be done after 6–12 months of therapy.
Future prospects
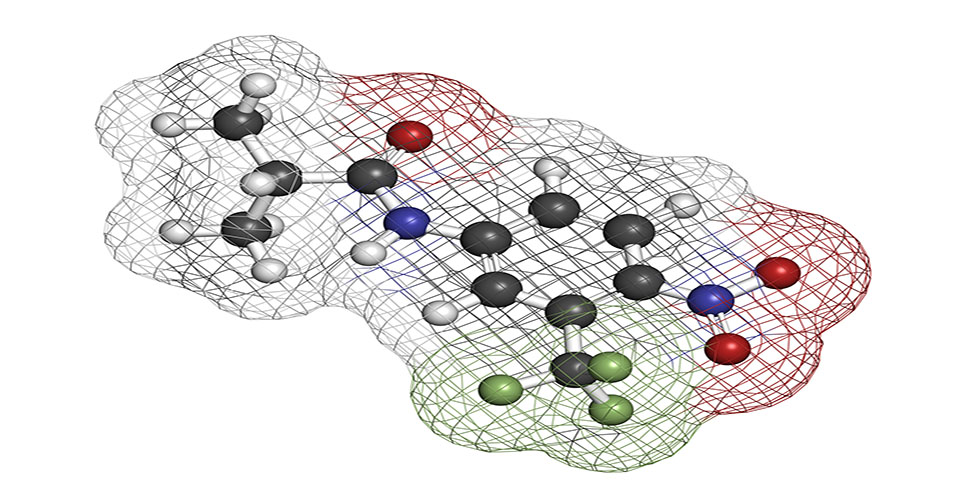
Orally active selective androgen receptor modulators (SARMS) represent an attractive approach to androgen replacement therapy in male hypogonadism. They target the androgen receptor in different tissues in a different manner in order to elicit the desired effects on bone, muscle, CNS, etc, without adversely affecting other organs (eg, prostate, liver or breast).
Moreover, the development of molecules with distinct tissue specificity could provide the rationale for their use for indications well beyond hypogonadism (eg, osteoporosis in the elderly, anaemias, muscular wasting and cancer cachexia).
Further reading
Negro-Vilar A. Selective androgen receptor modulators (SARMs): a novel approach to androgen therapy for the new millennium. J Clin Endocrinol Metab 1999;84:3459-62.
Swerdloff RS, Wang C, Cunningham G, et al. Long-term pharmacokinetics of transdermal testosterone gel in hypogonadal men.
J Clin Endocr Metab
2000;85:4500-10.
Vermeulen A. Androgen replacement therapy in the aging male: a critical evaluation.
J Clin Endocr Metab
2001;86:2380-94.
AACE Hypogonadism Guidelines.
Endocr Pract 2002;8(6):447-56.