teaser
Lisa Licitra
MD
Head and Neck Medical Oncology Unit
Medical Oncology Department
Istituto Nazionale per lo Studio e la Cura dei Tumori
Milan
Italy
E:[email protected]
In 1995 in Europe there were about 72,000 new cases of head and neck squamous cell carcinomas (HNSCCs) and 31,000 deaths, making it the eighth leading cause of cancer death and the seventh for incidence.(1)
HNSCC arises from the mucosa of the upper aerodigestive tract, including cancers of the oral cavities, the pharynx (naso-, oro- and hypopharynx), the larynx and the paranasal sinuses.
Approximately 60–65% of patients with head and neck cancer can be cured with surgery and/or radiotherapy. Patients with early-stage disease (I and II) are treated with single-modality treatment (either surgery or radiotherapy), while patients with a more advanced disease (stages III and IV) need a combined approach, such as extensive surgery and radiotherapy or chemoradiation. In cases of advanced disease, the probability of cure fails to 30%. Causes for treatment failure are local regional recurrence (60%), followed by metastatic disease (up to 30%) and second primaries.(2)
Treatment of HNSCC
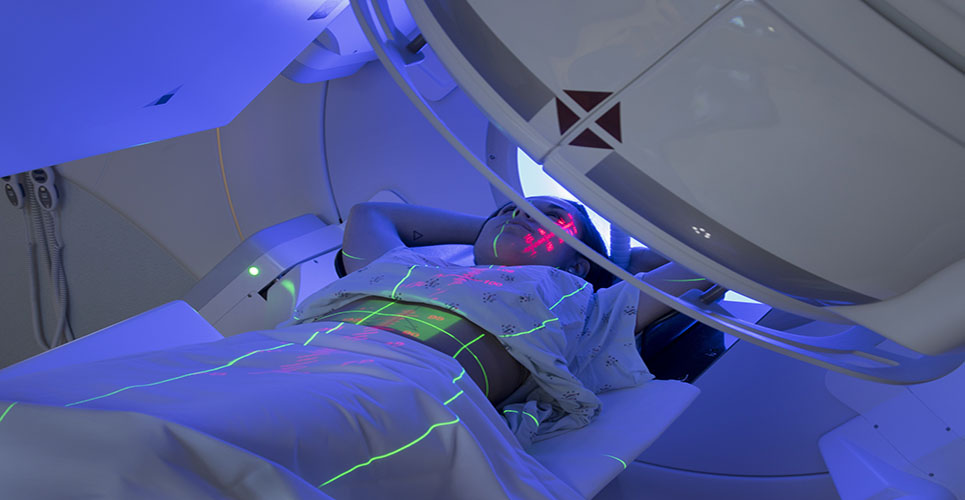
Radiotherapy
Advances in radiation therapy, particularly locoregional control, have recently been made by altering the conventional fractionation scheme.(3–6) These promising results explain why subsequent research has mainly focused on the association of chemotherapy with a nonconventional fractionation radiotherapy programme.
Chemotherapy for locally advanced HNSCC
The role of chemotherapy in advanced head and neck cancer is under continuous evaluation. Three meta-analyses have reviewed its use, and all three concluded that chemotherapy was associated with a statistically significant, although low, advantage in survival.(7–9) The latest meta-analysis was recently updated with individual data on patients enrolled in 24 new trials, most of them including some form of chemotherapy in addition to locoregional treatment, totalling 87 randomised trials and more than 16,000 patients.(10)
There was a significant improvement in overall survival in favour of chemotherapy compared with locoregional treatment alone, with a 12% reduction in the hazard ratio of death. This reduction corresponds to an absolute survival benefit of 5% at five years. The most important benefit was seen when chemotherapy was concomitantly given with radiation therapy. Other interesting observations were that the effect of concomitant chemotherapy was not dependent on whether polychemotherapy (eg, cisplatin + fluorouracil) or a single agent (eg, cisplatin or fluorouracil) was given. Moreover, the effect of chemotherapy on survival markedly decreased with increasing age (>60 years). Finally, there was no significant impact on death hazard ratio associated with sex, performance status (PS), stage and tumour site.
All treatment improvements were achieved at the expense of a significant increase in acute toxicity (mainly bone marrow), sometimes even leading to toxic deaths. Other local toxicities comprised dermatitis, mucositis or need for a feeding tube.
However, in these different studies, acute and late toxicities were reported according to different toxicity scales, thus preventing sound toxicity profile comparisons in an attempt to identify the schedule that minimises severe toxicity. Moreover, late toxicity is not systematically reported, although it seems to be slightly superior in the concomitant chemoradiation approach. Future research efforts should attempt to reduce morbidity of concurrent chemoradiation by optimal selection of radiation fractionation, drugs and scheduling, and by optimising supportive care.
Chemotherapy and radiation as adjuvant treatment after surgery
Based on the unsatisfactory results obtained by surgery and adjuvant radiotherapy in advanced high-risk patients, the role of concomitant chemoradiation as adjuvant treatment has been investigated. Two randomised trials addressing this issue have recently been published, revealing that cisplatin given at 100mg/m(2) every 21 days concurrently with postoperative radiation shows some benefit in the chemoradiation arm, compared with the postoperative radiation-alone arm. Both trials included operated head and neck cancer patients (defined as high-risk for locoregional recurrence according to specific risk factors, as discovered at the pathological examination of the surgical specimen), irrespective of tumour subsite.(11,12)
Novel agents in the treatment of recurrent and/or metastatic HNSCC
The standard of care for palliative management of recurrent and/or metastatic HNSCC has been either the combination of cisplatin and fluorouracil or a monochemotherapy with methotrexate or cisplatin. The combination offers a slightly superior response rate, which unfortunately does not translate into an improvement of survival over monochemotherapy alone, at the expense of more toxicity. Under these conditions, patients’ selection is important in order to maximise tumour response probability while minimising risk of toxicity.
With the advent of new molecularly targeted agents, such as epidermal growth factor receptor (EGFR) inhibitors, the number of therapeutic options in this field has increased. Targeting EGFR in HNSCC is a rational approach sustained by a large body of evidence. The high proportion of HNSCC overexpressing EGFR (80–100%) in an established tumour, as well as in normal mucosa of HNSCC patients, supports the relevance of the target. Moreover, its overexpression has been related to poor prognosis in patients with HNSCC, and, more recently, its prognostic role was more specifically related to the received treatment, such as radiotherapy(13,14) and chemotherapy.(15) Selective agents targeting EGFR are under clinical evaluation.(16) Among new compounds, the most advanced for the treatment of HNSCC is the monoclonal antibody C225 (Erbitux); two small-molecule EGFR-tyrosine kinase inhibitors, ZD1839 (gefitinib; Iressa) and OSI-774 (erlotinib; Tarceva), are also being investigated. The results of the studies employing these new agents are reported in Tables 1 and 2.
[[HPE21_table1_68]]
[[HPE21_table2_68]]
Erbitux has been successfully employed in a phase III trial investigating radiation therapy alone versus radiation in combination with weekly administration of the drug. The trial showed improved survival rates in the experimental arm, and, interestingly, this was associated with limited acute toxicity, which was not superior to that observed in the standard radiation arm.(17) Erbitux has also been studied in combination with cisplatin or carboplatin in patients progressing under cisplatin, with a progression rate of 14%.(18) In another phase III trial, the drug was associated to cisplatin as first-line treatment. Preliminary data showed no benefit in the experimental arm in terms of progression-free survival, despite an improvement in response rate, from 10% to 20%.(19)
In general, objective tumour response rate with these new agents is poor, although progression-free survival in both trials is encouraging, as the anticipated effect of these cytostatic compounds was disease stabilisation. It is worth pointing out that, in both studies, skin toxicity was associated with better survival.
References
- Ferlay J, et al. Cancer incidence, mortality and prevalence worldwide, version 1.0. Lyon: IARC Press. IARC Cancer Base No. 5.2001
- N Engl J Med 1993;328:184-94.
- Int J Radiat Oncol Biol Physics 2000;48:7-16.
- Lancet 2003;362:933-40.
- Radiother Oncol 1992:25:231-41.
- Radiother Oncol 1997;44:111-21.
- Br J Cancer 1995;71:83-91.
- J Clin Oncol 1996;14:838-47.
- Lancet 2000;355:949-55.
- J Clin Oncol 2004;22 Suppl:Abstract 5505.
- N Engl J Med 2004;350:1937-44.
- N Engl J Med 2004;350:1945-52.
- Cancer Res 2002;62:7350-6.
- Int J Radiat Oncol Biol Phys 2004;58:561-6.
- Head Neck 1991;13:132-9.
- Crit Rev Oncol Hematol 2005;53:179-92.
- J Clin Oncol 2004;22 Suppl:Abstract 5507.
- Proc Am Soc Clin Oncol 2002;21:Abstract 900.
- Proc Am Soc Clin Oncol 2002;21:Abstract 901.
- Proc Am Soc Clin Oncol 2002;21:Abstract 925.
- J Clin Oncol 2004; 22 Suppl:Abstract 5502.
- J Clin Oncol 2005;23:epub 04/04/2005 (10.1200/JCO.2005.02.147).
- J Clin Oncol 2004;22 Suppl:Abstract 5513.
- J Clin Oncol 2004;22 J Clin Oncol 2005;23:epub 04/04/2005 (10.1200/JCO.2005.02.147).
- J Clin Oncol 2004;22 Suppl:Abstract 5539.
- J Clin Oncol 2004;22 Suppl:Abstract 5540
- J Clin Oncol 2003;21:1980-7.
- J Clin Oncol 2004;22 Suppl:Abstract 5586.
- J Clin Oncol 2004;22:77-85.