AI model has been shown to be able to predict 10-year incident MACE with similar performance to the established clinical standard
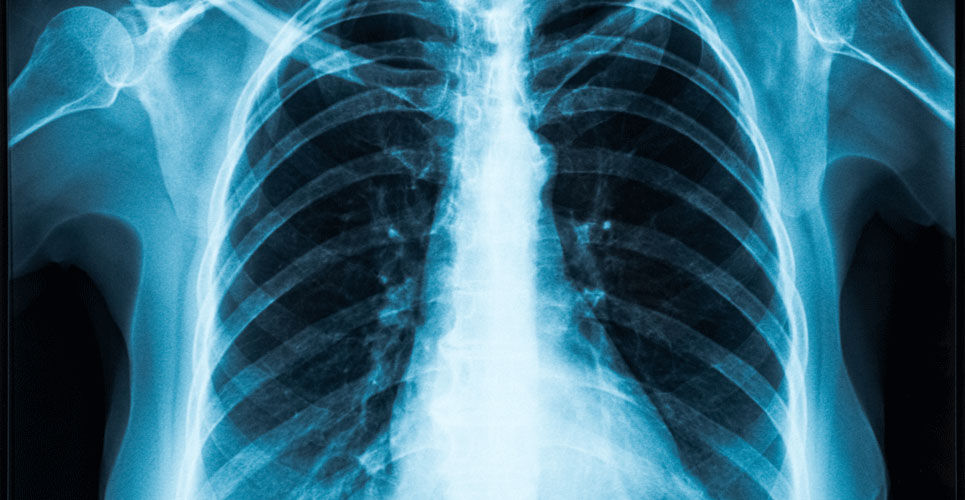
The use of an AI model which utilises data derived from a single chest X-ray, is able to predict the 10-year risk of death from a heart attack or stroke, stemming from atherosclerotic cardiovascular disease (ASCVD) according to the results of a study presented at the Radiological Society of North America (RSNA) conference 2022.
The term ‘deep learning’ refers to a subset of machine learning, which is essentially a neural network with three or more layers which attempt to simulate the behaviour of the human brain — albeit far from matching its ability—allowing it to “learn” from large amounts of data. Among patients with cardiovascular disease, risk assessment is a critical step in the current approach to primary prevention of atherosclerotic cardiovascular disease (ASCVD). Knowledge of the 10-year risk for atherosclerotic cardiovascular disease identifies patients in higher-risk groups who are likely to have greater net benefit and lower number needed to treat for both statins and antihypertensive therapy. The current assessment of risk relies on a limited set of risk factors, namely, age, sex, systolic blood pressure, antihypertensive treatment, total and HDL-cholesterol, diabetes, and cigarette smoking. However, according to Jakob Weiss, a radiologist affiliated with the Cardiovascular Imaging Research Center at Massachusetts General Hospital and who was involved in the RSNA study, ‘variables necessary to calculate ASCVD risk are often not available, which makes approaches for population-based screening desirable adding that, ‘as chest X-rays are commonly available, our approach may help identify individuals at high risk.’
In the current study, Dr Weiss and his team, developed the AI model (referred to as CXR-CVD) using 147,497 chest radiographs (CXR) from 40,643 participants from the PLCO cancer screening trial and which was trained to predict cardiovascular mortality from a single CXR image. In addition, the team undertook independent testing in a second separate cohort of 11,430 outpatients potentially eligible for primary prevention and with no prior major adverse cardiovascular events (MACE). The prognostic value of the AI model was compared to the established ASCVD risk score in a subset of 2,401 (21%) patients and for whom, the variables necessary to calculate ASCVD risk were available. The primary outcome was observed 10- year incident MACE and both hazard ratios (HR) and c-statistics were estimated using Cox proportional hazards regression.
AI Model prediction of cardiovascular risk
A total of 11,430 patients with a mean age of 60.1 years (42.9% male) were included in the independent testing dataset. Over a median follow-up of 10.3 years, there were 9.6% MACE events documented.
Using the AI model, there was a significant association with MACE in statin eligible patients (HR = 2.03, 95% CI 1.81 – 2.30, p < 0.001) and after adjustment for cardiovascular risk factors, this association remained significant (HR = 1.63, 95% CI 1.43 – 1.86, p < 0.001).
In the subgroup of patients for whom all the necessary ASCVD variables were available, the performance of the AI model was similar (c-statistic = 0.64 vs. 0.65; p = 0.48) to but also additive to, the ASCVD risk score (HR = 1.58, 95% CI 1.20 – 2.09, p = 0.001).
The authors concluded that using a single routine CXR image, the AI model was able to predict 10-year incident MACE with similar performance and incremental to the established clinical standard. They added that since CXR images are commonly available, our approach may help identify individuals at high risk for cardiovascular disease, prompting risk factor assessment and targeted prevention.
Citation
Weiss J et al. Deep Learning to Predict 10-year Cardiovascular Risk from Chest Radiographs. Presented at the RSNA 2022.