Addition of coronary artery calcium scores to a patient’s cardiovascular risk assessment provides little meaningful benefit, according to a recent study
Coronary artery calcium scores (CACS) added to an individual’s cardiovascular risk assessment is not associated with any meaningful clinical benefit. This was the conclusion from a systematic review and meta-analysis by a team from the School of Public Health, University of Sydney, Sydney, Australia.
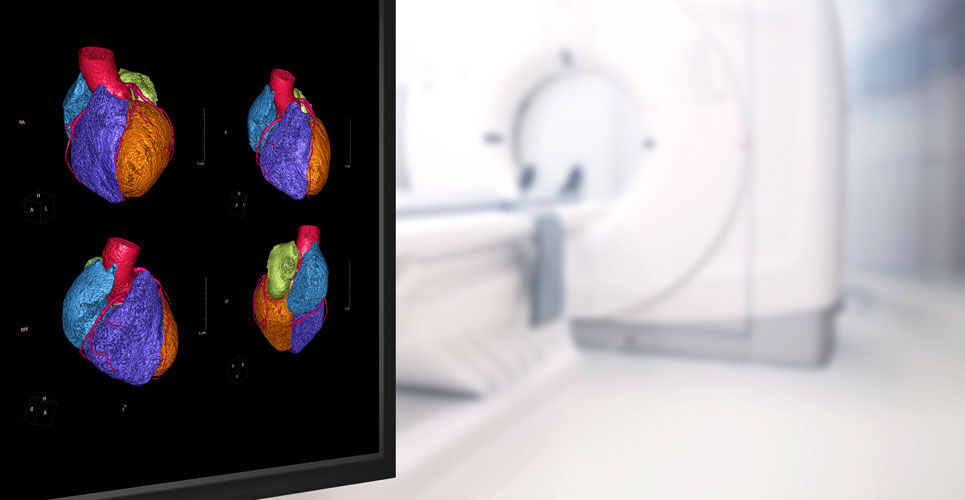
A critical step in primary prevention of heart disease is an assessment of a patient’s cardiovascular risk and can be calculated using tools such as QRISK. The use of cardiac computed tomography (CT) imaging is an important tool for cardiovascular risk assessment in observational prospective studies, providing measures of subclinical disease such as coronary artery calcium score (CACS). In fact, use of CACS has been shown to be an independent predictor of incident coronary heart disease among those deemed to be at intermediate-risk based on their Framingham risk score. Furthermore, CACS screening has been found to improve medication adherence and provide superior coronary artery disease risk factor control without increasing downstream medical testing. However, not all research has come to the same conclusion with a study in post-menopausal women concluding that there was no independent benefit of coronary CT imaging in a low-to-moderate risk group.
With a degree of uncertainty over whether addition of CACS derived from CT imaging provides an incremental benefit beyond that obtained from traditional risk assessment methods, in the current study, the Australian team undertook a systematic review and meta-analysis of available studies. They included studies in patients without existing cardiovascular disease, where at least one recognised risk calculator and a CACS had been used. The primary outcome as the change in C statistic for a model which contained the CACS compared to the base model without the CACS.
Coronary artery calcium scores and improvement in CVD risk prediction
A total of 6 studies with 17,961 individuals and 1043 cardiovascular events were included in the analysis. The studies varied in sample size from 470 to 5185 and mean ages ranged from 50 to 75.1 years (38.4 to 59.4% female).
The C statistic for cardiovascular disease (CVD) risk models but without CACS ranged from 0.693 to 0.80. Inclusion of CACS improved the pooled C statistic by 0.036.
When CACS was added, among participants whose risk was reclassified from low to intermediate or high risk, 85.5% to 96.4% did not experience an event during follow-up (ranging from 5.1 to 10 years). Among those who were reclassified from high risk to low risk by CACS, a similarly high proportion, 91.4% to 99.2% did not have a CVD event during follow-up.
The authors suggested that while CACS did appear to provide modest further discriminatory power to traditional risk factor assessments, this additional gain needed to be balanced against the higher costs and radiation risks. They concluded that while there were gains from inclusion of CACS, which patients might benefit remains to be determined and that there is no evidence to suggest that use of CACS offers a clinical benefit.
Citation
Bell KJL et al. Evaluation of the Incremental Value of a Coronary Artery Calcium Score Beyond Traditional Cardiovascular Risk Assessment: A Systematic Review and Meta-analysis JAMA Intern Med 2022