Rezafungin (brand name Rezzayo) has been approved by the European Commission for the treatment of invasive candidiasis in adults, its manufacturer Mundipharma has announced.
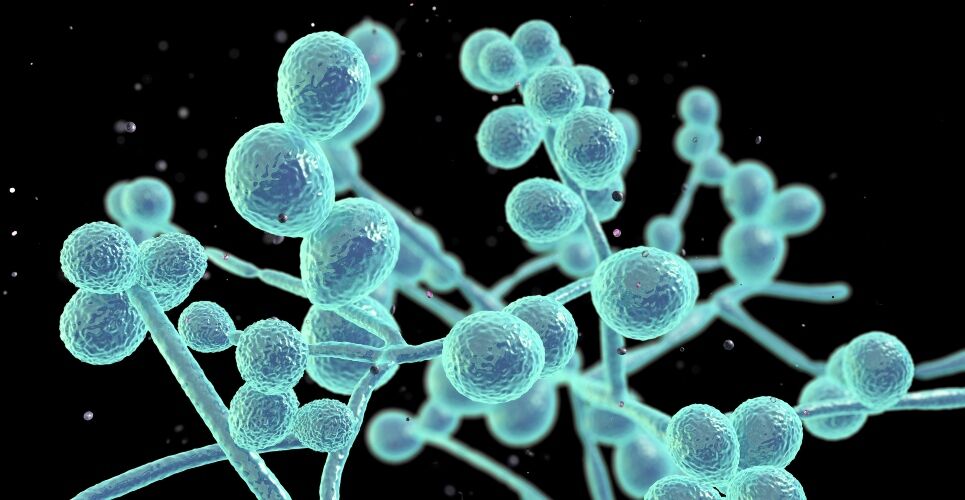
An antimycotic, rezafungin selectively inhibits the fungal enzyme 1,3-β-D-glucan synthase, inhibiting formation of 1,3-β-D-glucan, an essential component of the fungal cell wall. This, in turn, results in rapid and concentration-dependent fungicidal activity in Candida species.
The first new treatment option in over 15 years for patients with invasive candidiasis, rezafungin has been granted orphan drug designation and will be available as a 200 mg powder for concentrate for solution for infusion.
Professor Oliver Cornely, head of the European Excellence Centre for Medical Mycology at the University Hospital Cologne, Germany, said: ‘There has been a significant global unmet need for treating people with invasive candidiasis. [This] announcement by the European Commission marks an important moment that could enable the healthcare professional community to manage invasive candidiasis patients in a different way using a new treatment option.’
Despite a number of available treatments, the mortality rate for patients with invasive candidiasis is as high as 40% or more.
Rezafungin non-inferior to caspofungin
The approval follows the positive opinion of the Committee for Medicinal Products for Human Use in October 2023 and is based on results from the pivotal ReSTORE Phase III clinical trial, for which Professor Cornely was a data review committee member.
This multicentre, double-blind, double-dummy, randomised trial compared the efficacy and safety of intravenous rezafungin compared with intravenous caspofungin – the current standard of care – in patients with candidaemia and invasive candidiasis.
The primary endpoint relevant for the EU approval was global cure (consisting of clinical cure, radiological cure and mycological eradication) at day 14 with a target non-inferiority margin of 20%, assessed in the modified intention-to-treat population.
Of the 222 patients screened for inclusion, 199 were deemed eligible and 100 were randomly assigned to the rezafungin group and 99 to the caspofungin group.
Some 59% of patients in the rezafungin group and 61% of patients in the caspofungin group had a global cure at day 14 (weighted treatment difference −1·1% [95% CI −14·9 to 12·7].
The trial therefore demonstrated statistical non-inferiority for rezafungin, dosed once weekly, when compared to caspofungin dosed once daily.
The most common treatment-emergent adverse events that occurred in at least 5% of patients in either group were pyrexia, hypokalaemia, pneumonia, septic shock and anaemia.
The findings are supported by the positive results of the STRIVE Phase II clinical trial and an extensive non-clinical development program.