Donanemab has been shown to clear more brain amyloid than aducanumab in a head-to-head study in patients with early Alzheimer’s disease
According to the drug manufacturer Lilly, donanemab gives rise to a greater reduction in the level of brain amyloid clearance compared to aducanumab at six months.
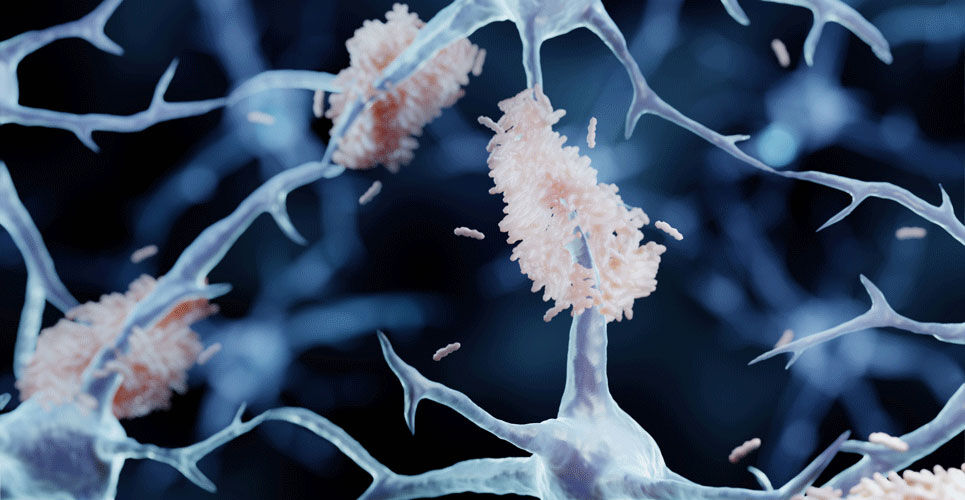
Brain amyloid-β deposition is a hallmark used to define Alzheimer’s disease. Moreover, in March 2022, the Food and Drug administration (FDA) in the US, approved the first in vitro diagnostic test for early detection of amyloid plaques associated with Alzheimer’s disease. The FDA added that a positive test was consistent with the presence of amyloid plaques, similar to what would be seen in a PET scan and that a negative result is consistent with a negative amyloid PET scan result, reducing the likelihood that a patient’s cognitive impairment was due to Alzheimer’s disease, enabling physicians to pursue other causes of cognitive decline and dementia.
The current data announced by Lilly, comes from the TRAILBLAZER-ALZ 4 trial, which was a randomised, open-label phase 3 study designed to compare donanemab (DM) with aducanumab (AM) on amyloid plaque clearance in participants with early, symptomatic Alzheimer’s Disease. In the trial, donanemab and aducanumab were administered via intravenous infusions every four weeks for up to 18 months.
Donanemab efficacy
In the co-primary outcomes, brain amyloid plaque clearance, defined as achieving brain amyloid plaque levels of <24.1 Centiloids, was achieved in 37.9% of DM-treated participants compared with 1.6% of AM-treated patients at six months. In the intermediate tau subpopulation, 38.5% of DM-treated participants reached brain amyloid clearance compared with 3.8% of AM-treated participants by six months. In a key secondary outcome, DM reduced brain amyloid levels vs. baseline by 65.2% compared with 17.0% for AM at 6 months. In an exploratory outcome, donanemab, but not aducanumab treatment significantly reduced plasma P-tau217 at six months compared to baseline.
In terms of safety, amyloid-related imaging abnormalities were the most common treatment emergent adverse event in both groups and occurred with a similar frequency (25.4% vs 26.1%, DM vs AM).
Although only six-month data is currently available, TRAILBLAZER-ALZ 4 is an ongoing study and results from 12 or 18 months will be presented once available.