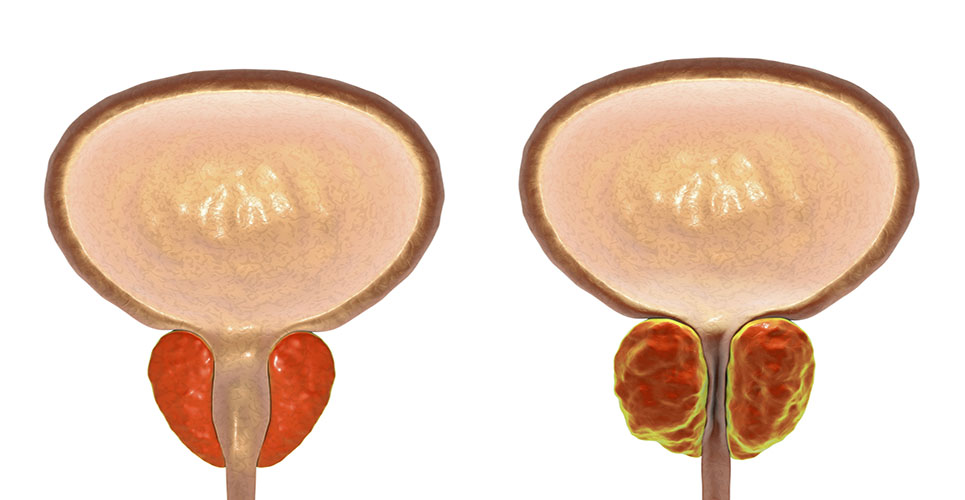
For men who develop hormone-resistant prostate cancer (HRPC), currently licensed therapies are largely palliative and often toxic.
The use of immunotherapy is attractive in HRPC, as the patient’s immune system often remains robust and treatment toxicity is low. The aim of immunotherapy in HRPC is to maintain quality of life and convert a terminal disease to a chronic, “managed” disease state.
The manipulation of the patient’s immune system to attack his/her own cancer has recently gathered pace within the commercial sector (see Table 1).
[[HPE28_table1_23]]
Onyvax Ltd, a London-based biopharmaceutical company, is continuing to develop ONY-P, which are combinations of nonpatient-specific prostate cancer cell lines taken from different disease stages and mixed with BCG as a general immune system activator/adjuvant, for the treatment of HRPC.(1,2)
Translation from tissue donor to industrial manufacture of product
The isolation and subsequent conversion of human cells to therapeutic candidate is not a trivial undertaking. Donor tissue must meet stringent criteria that cover procedures for donation, procurement and testing for communicable disease.(3–5) Following in-vitro tissue culture, the resulting cell lines need to be characterised not only for suitable phenotype (eg, expression of known tumour-associated antigens and proteins indicative of local or metastatic disease), but also the ability to grow under industrial manufacturing conditions. With the publication of the EU Directive on Clinical Trials,(6,7) all clinical trial material has to be manufactured to current good manufacturing practice (GMP) to ensure they are of the appropriate quality to protect trial participants. Clearly, the ability to construct a manufacturing process early in the development chain that is scaleable and can be executed in an industrial setting is highly important. For ONY-P, disposable, presterilised multilayer growth vessels are used to produce the cell bulk as they have the advantages of being modular, therefore amenable to scale-up, and reduce the need for costly cleaning and sterilisation procedures associated with more standard reuseable bioreactor systems.
Product safety and quality must be maintained up to patient administration. Like other complex biologicals, ONY-P requires an extensive cold chain. To maintain product integrity, Onyvax provides clinical trial sites with –80°C freezers and training for the storage, thawing and preparation of product for administration.
Clinical trial challenges
Historically, the primary endpoint of oncology clinical trials, which often take years to complete, was overall survival. Pressure from governments, industry and most importantly patients has driven recent initiatives to reduce development time. These are exemplified by the FDA’s Critical Path initiative,(8) which looks to promote the use of novel study designs and interim data analysis, often using surrogate endpoints (eg, tumour response to therapy). These more flexible designs can reduce patient numbers, which is ethically attractive (see Table 2).
[[HPE28_table2_24]]
Conventional oncology surrogate endpoints (eg, tumour response rates)(9,10) are not always appropriate for immunotherapies that may not reduce tumour burden but slow down disease progression. Onyvax has employed both progression-free survival (PFS) and biomarkers as surrogate endpoints. Biomarkers show huge promise for the expedition of trials by predicting treatment responses prior to survival endpoint. Additionally, they may allow better selection of patients so nonresponders can be moved quickly to alternative therapy. ONY-P1 (Onyvax’s lead candidate) has been shown to affect the rate of increase of the blood biomarker prostate-specific antigen (PSA) in 42% of treated HRPC patients.(2) In addition, the median PFS was 58 weeks in treated individuals, compared with historical controls of around 28 weeks. Although PSA is not currently a validated surrogate endpoint for product licensure, as definitive clinical correlation to a survival endpoint is lacking, PFS is accepted by regulatory authorities. These observations hold out the promise of using PSA for interim analyses in adaptive study designs.
Onyvax is also investigating immune-response biomarkers. Conventional statistical approaches have not been sufficient to correlate any immune biomarker(s) with clinical outcome, so an artificial neural network has been utilised to mine the dataset.(2) Following analysis of 20,000 datapoints, a panel of potential biomarkers has been identified for further investigation in ONY-P clinical trials.
Next steps
ONY-P is about to enter a randomised, double-blind, placebo-controlled phase IIb trial with PSA interim analysis in HRPC patients. The primary study objective is to confirm treatment efficacy against placebo using a vaccine manufactured under large-scale commercial conditions, and to evaluate immune-response biomarkers further. ONY-P is well placed to utilise the current drive within both the regulatory and industry spaces to move away from classic clinical approaches and, where appropriate, embrace more flexible and creative thinking to bring innovative medicine quickly and safely to patients with unmet clinical need.
Authors
Stephen John Ward PhD
Head of Process Development
Christopher Beattie MBA
Head of Development
Onyvax Ltd
St George’s Hospital Medical School, London, UK
E:[email protected]
References
1 Eaton JD, Perry MA, Nicholson S, et al. Allogeneic whole-cell vaccine: a phase I/II study in men with hormone-refractory prostate cancer. BJU Int 2002;89:19-26.
2 Michael A, Ball G, Quatan Nadine, et al. Delayed disease progression after allogeneic cell vaccination in hormone-resistant prostate cancer and correlation with immunologic variables. Clin Cancer Res 2005;11:4469-78.
3 US Food and Drug Administration. 21CFR Part 1271 – Good tissue practice final rule; May 2005.
4 Directive 2004/23/EC of the European Parliament and of the Council March 2004.
5 UK Human Tissue Act 2004.
6 Directive 2001/20/EC of the European Parliament and of the Council; May 2001.
7 UK Statutory Instrument 2004 No. 1031. The medicines for human use (clinical trials) regulations 2004;May 2004.
8 US Food and Drug Administration. Critical path initiative; the critical path to new medicinal products. Initiated March 2004.
9 Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumours. J Natl Cancer Inst 2000;92:205-16.
10 WHO handbook for reporting results of cancer treatment. Geneva (Switzerland): World Health Organization Offset Publication 1 1979; 48.