Cambridge scientists have shown how the lubricant that ordinarily allows our joints to move smoothly triggers a pain response from nerve cells in osteoarthritis.
In recent years it has become clear that osteoarthritis is not restricted to cartilage damage, but is a failure of the entire joint, with inflammation – the body’s response to stress and injury – being a major contributor to the pain experienced by patients. A recent collaboration between the two pharmaceutical companies Pfizer and Eli Lilly has found that their anti-inflammatory drug, tanezumab, produced pain relief for osteoarthritic patients in a Phase III clinical trial.
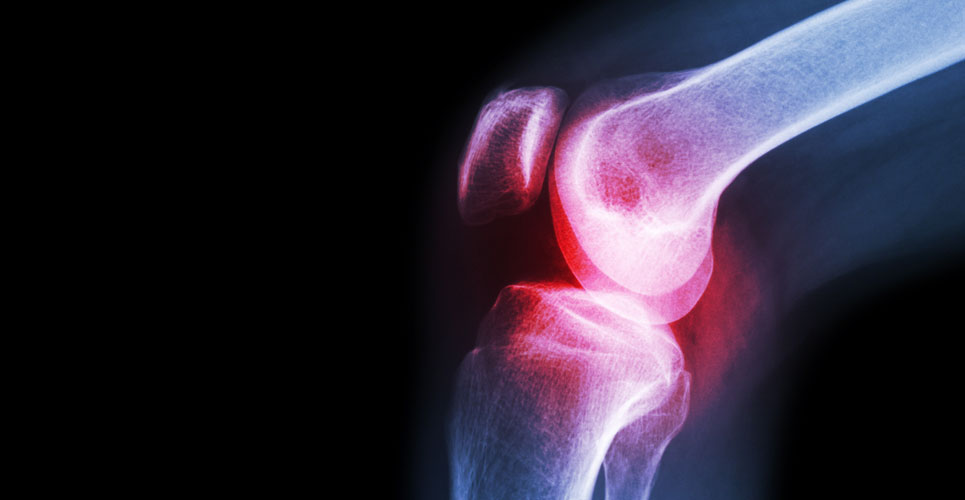
When inflammation occurs during osteoarthritis, the body produces an increased number of cells within and around the joint. These cells release inflammatory substances into the synovial fluid, the lubricant that allows joints to move smoothly. During osteoarthritis, synovial fluid becomes less viscous and these inflammatory substances come into direct contact with sensory nerve cells in the joint, producing the sensation of pain.
In a study published in the journal Rheumatology on 13 August 2019, researchers at the University of Cambridge and Addenbrooke’s Hospital, part of Cambridge University Hospitals, examined whether synovial fluid produced during osteoarthritis is capable of directly exciting sensory nerves supplying knee joints – those nerves responsible for transmitting pain signals.
“Osteoarthritis can be a very painful condition, but we only know a little about what causes this pain,” says Sam Chakrabarti, a Gates Cambridge Scholar. “We wanted to investigate what was happening in the joint and to see whether it was the lubricant that ordinarily keeps these joints moving that was contributing to the pain. Studies such as these are important in helping us develop better treatments.”
The researchers obtained synovial fluid from consenting osteoarthritis patients at Addenbrooke’s Hospital and from post-mortem donors with no known joint disease. They then incubated knee sensory nerves isolated from mice in either healthy or osteoarthritis synovial fluid and recorded the activity of these nerves.
The team found that when incubated with osteoarthritic synovial fluid, the knee nerves were more excitable. The nerves also showed an increase in the function of TRPV1, a molecule that detects the hotness of chilli peppers (TRPV1 is also activated by heat, which is why chillis tastes hot). Although the presence of inflammatory chemicals in osteoarthritis synovial fluid has been known since 1959, this is the first evidence that synovial fluid can directly excite sensory nerves and hence is an important contributor to an individual’s experience of pain.
“This is the first time we have been able to use synovial fluid from human osteoarthritis patients to excite sensory nerve cells, making it more clinically-relevant than mouse studies alone, and so will hopefully help translating treatments from bench to bedside,” says Dr Ewan St John Smith from the Department of Pharmacology at the University of Cambridge.
“In the future, this set up can be used to identify the specific components of synovial fluid that cause pain and then to test if and how a drug will be useful in arthritic pain. Since synovial fluid is regularly collected from arthritic patients as part of their treatment regime, our technique can be easily set up in laboratories throughout the world to understand and help to identify a cure for arthritic pain.”
Dr Deepak Jadon, Director of the Rheumatology Research Unit at Cambridge University Hospitals, adds: “This study highlights how much we can learn with the help of our patients, as well as the importance of collaboration between clinicians and basic scientists.”
Reference
Chakrabarti S et al. Human osteoarthritic synovial fluid increases excitability of mouse dorsal root ganglion sensory neurons: an in-vitro translational model to study arthritic pain. Rheumatology;13 August 2019;DOI: 10.1093/rheumatology/kez331