Pierre D Delmas
MD PhD
President
International Osteoporosis Foundation
Professor of Medicine
A Fontana
MD
Department of Rheumatology and Bone Diseases
Edouard Herriot Hospital
Lyon, France
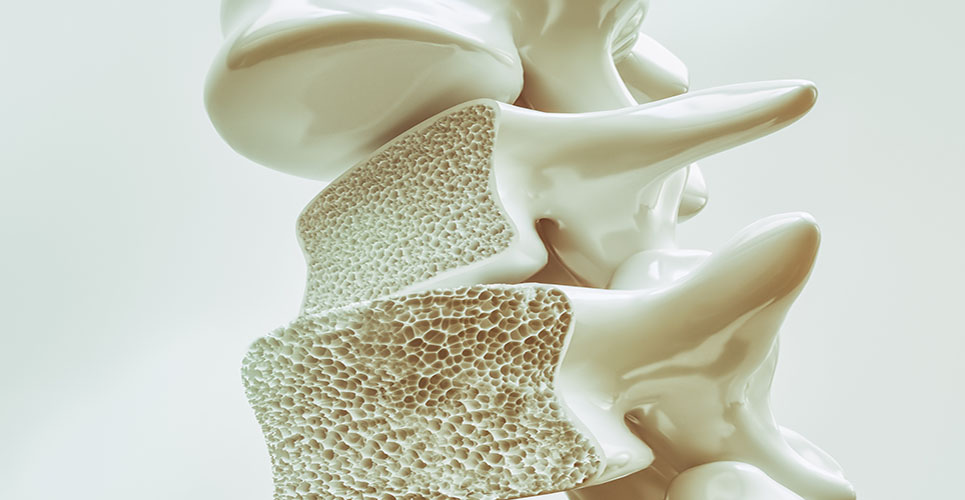
Osteoporosis is a disease characterised by a low bone mass and a deterioration of bone architecture leading to an increased risk of fracture. Fragility fractures occur after a small trauma at any skeletal site, most commonly at the hip, the spine or the wrist, and they are associated with increased morbidity and mortality. In postmenopausal osteoporosis, the most common form of the disease, there is an increased rate of bone turnover with an increase in bone resorption (degradation) relative to bone formation.
Bisphosphonates are molecules with a strong affinity for bone mineral that markedly inhibit t he activity of osteoclasts, the cells responsible for bone resorption. They are widely used in a variety of conditions associated with increased bone resorption, such as hypercalcaemia, multiple myeloma, bone metastases and Paget’s disease of bone. They have recently become a first-line therapy for postmenopausal osteoporosis.
Features common to bisphosphonates
Bisphosphonates are poorly absorbed by the gut (around 1% for most of them), with major food and calcium interaction, and need to be taken on an empty stomach with water. About half of absorbed bisphosphonate is retained in the skeleton, and the other half is cleared through the kidney. The safety profile of bisphosphonates is favourable. The possibility of minor gastrointestinal discomfort has been reported for all bisphosphonates (such as dyspepsia, abdominal pain and diarrhoea), but this rarely leads to discontinuation. Rare cases of oesophagitis have been reported with alendronate. Etidronate can induce a mineralisation defect of bone after prolonged use, but this has not been seen with other bisphosphonates.
Etidronate
Etidronate was the first bisphosphonate to be developed. Etidronate 400mg per day, for 15 days every three months, is indicated in the treatment of osteoporosis. Two placebo-controlled studies have shown small increases in bone mineral density (BMD) at the lumbar spine with a significant reduction in vertebral fractures.(1,2) However, the reduction in vertebral fractures after two years of treatment was not sustained after three years. Etidronate does not reduce the risk of hip fracture.
Alendronate
A dose-dependent increase in spine BMD has been reported in postmenopausal women with low BMD treated with alendronate. Compared with placebo after two years of treatment, the 10mg/day dose induced an increase of 8.6% and 6.5% in the lumbar spine and total hip BMD, respectively.(3)
A study (FIT-1) in 2,027 osteoporotic women with at least one prevalent vertebral fracture treated with alendronate 5mg daily for two years, followed by 10mg daily during a third year, demonstrated a significant 50% reduction in vertebral, wrist and hip fractures compared with placebo.(4)
Women with a low BMD but without vertebral fracture at baseline (FIT-2) were treated with alendronate for four years using the same placebo-controlled design. There was a small decrease in clinical fracture incidence with alendronate that did not reach significance (p = 0.07).(5) The incidence of new vertebral fractures, as defined by morphometry, was significantly reduced by treatment. When the analysis was restricted to those patients that had osteoporosis according to the WHO criteria – a BMD more than 2.5 standard deviations below the mean value of healthy premenopausal women (T-score ≤2.5) – the reduction in all types of clinical fractures was significant.
Finally, a placebo-controlled study in 1,908 postmenopausal women with low BMD (T-score <–2) showed a 47% reduction in the risk of non-vertebral fractures after one year of alendronate 10mg/day.(6)
In a study of 1,174 postmenopausal women under 60 years of age or younger, alendronate 5mg/day induced at two years a significant increase of 3.5% and 1.9% in lumbar spine and hip BMD, respectively, compared with placebo.(7) Alendronate is approved for the treatment of osteoporosis at a daily dose of 10mg and for the prevention of osteoporosis at a daily dose of 5mg.
The efficacy of alendronate 10mg/day has been demonstrated in a two-year double-blind placebo-controlled trial of 241 men with osteoporosis (T-score at the femoral neck ≤–2 or ≤–1 with a fragility fracture).(8) The increase in BMD was comparable to that in women, and the incidence of vertebral fractures was significantly decreased in the alendronate group compared with the placebo group (0.8% versus 7.1%).
It has been shown that alendronate given once a week at a dose of 70mg has the same efficacy as 10mg daily to increase BMD and reduce bone turnover with an excellent safety profile.(9) In those countries in which it is available, the once-weekly regimen is extremely successful.
Risedronate
Two large trials have assessed the ability of risedronate to decrease the risk of new vertebral fractures among postmenopausal osteoporotic women with prevalent fractures in the USA(10) and in Europe and Australia.(11) The American study enrolled over 2,400 women and randomly assigned them to risedronate 2.5mg/day, 5mg/day or placebo. The 2.5mg group was discontinued after one year, and the other two groups were treated for three years. Risedronate 5mg/day significantly reduced the cumulative incidence of new vertebral fractures by 41% over three years, and by 65% after the first year. Non-vertebral fractures were significantly reduced by 39%. There was a significant increase in BMD in the 5mg/day group compared with placebo (5.4% at the lumbar spine, 1.6% at the femoral neck and 3.3% at the trochanter).(9)
The European and Australian study included 1,226 patients with at least two prevalent vertebral fractures.(11) The vertebral fracture reduction was 49% after three years of 5mg/day risedronate. The overall incidence of non-vertebral fractures in both studies was 30–40% lower in women treated with risedronate than in those treated with placebo.
The effects of risedronate on hip fractures has been assessed in 5,445 women aged 70–79 years with osteoporosis defined by a low BMD, and in 3,886 women over 80 years of age that were mainly recruited on the basis of clinical risk factors for falls, without BMD measurement for most of them.(12) The two groups were randomly assigned to receive risedronate 2.5mg/day, 5mg/day or placebo for three years. The overall analysis showed a 30% significant reduction of hip fractures (p = 0.02) with risedronate. In the first group, the reduction of hip fractures was larger (40%), reaching 60% in those with prevalent vertebral fractures. In contrast, there was no significant reduction in the second group, stressing the need to target bisphosphonates to those women who have osteoporosis as confirmed by BMD measurement.
Other bisphosphonates
Clodronate
Clodronate was developed over 20 years ago and is still widely used for the treatment of malignant bone diseases. In a study of 677 patients with osteoporosis (postmenopausal osteoporosis, secondary osteoporosis and men with osteoporosis), clodronate 800mg/day for three years decreased the incidence of new vertebral fractures by 46% (p = 0.07) compared with the placebo group.(13)
Tiludronate
Tiludronate is a bisphosphonate used in several countries for the treatment of Paget’s disease of bone. Its development in osteoporosis has been discontinued because of the lack of evidence of fracture reduction in large phase III trials at the dose tested.
Pamidronate
Oral daily pamidronate is probably effective in osteoporosis but is associated with a high incidence of upper gastrointestinal adverse events.(14) Intravenous infusion of pamidronate, commonly used in malignant bone disease and in Paget’s disease of bone, is used in some osteoporosis patients every three months.
Ibandronate
Ibandronate, another potent bisphosphonate, is currently under phase III investigation.
Conclusion
Bisphosphonates play a major role in the treatment of postmenopausal osteoporosis, with alendronate and risedronate being registered in most (if not all) European countries for the treatment of postmenopausal osteoporosis. Bisphosphonates are also likely to be used in the treatment of male osteoporosis and represent an alternative for younger postmenopausal women who cannot or do not want to use hormone replacement therapy.
Osteoporosis is a chronic disease that requires long-term therapy, but the optimal duration of bisphosphonate therapy is not known. The possibility of administering bisphosphonates intermittently will probably increase their long-term compliance.
References
- Storm T, Thamsborg G, Steiniche T, Genant HK, Sorensen OH. Effect of intermittent cyclical etidronate therapy on bone mass and fracture rate in women with postmenopausal osteoporosis. N Engl J Med 1990;322:1265-71.
- Watts NB, Harris ST, Genant HK, et al. Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N Engl J Med 1990;323:73-9.
- Chesnut CH, McClung MR, Ensrud KE, et al. Alendronate treatment of postmenopausal osteoporotic women: effect of multiple dosages on bone mass and bone remodelling. AJM 1995;99:144-52.
- Black DM, Cummings SR, Karpf DB, et al. Randomized trial of effect of alendronate on risk fracture in women with existing vertebral fractures. Lancet 1996; 348:1535-41.
- Cummings SR, Black DM, Thompson DE, et al. Effect of alendronate on risk fracture in women with low bone density but without vertebral fracture. JAMA 1998;280:2077-82.
- Pols HAP, Felsenberg D, Hanley DA, et al. Multinational, placebo-controlled, randomised trial of the effects of alendronate on bone density and fracture risk in postmenopausal women with low bone mass: results of the FOSIT study. Osteoporosis Int 1999;9:461-8.
- Hosking D, Chilvers CED, Christiansen C, et al. Prevention of bone loss with alendronate in postmenopausal women under 60 years of age. N Engl J Med 1998;338:485-42.
- Orwoll E, Ettinger M, Weiss S, et al. Alendronate for the treatment of osteoporosis in men. N Engl J Med 2000;343:604-10.
- Schnitzer T, Bone HG, Crepaldi G, et al. Therapeutic equivalence of alendronate 70mg once-weekly and alendronate 10mg daily in the treatment of osteoporosis. Alendronate Once-weekly Study Group. Aging (Milano) 2000;12:1-12.
- Harris ST, Watts NB, Genant HK, et al. Effects of risedronate treatment on vertebral and non-vertebral fractures in women with postmenopausal osteoporosis. A randomised controlled trial. JAMA 1999; 282:1344-52.
- Reginster JY, Minne HW, Sorensen OH, et al. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Osteoporosis Int 2000;11:83-91.
- McClung MR, Geusens P, Miller PD, et al. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 2001;344:333-40.
- McCloskey EV, Selby P, de Takats D, et al. Effects of clodronate on vertebral fracture risk in osteoporosis: a 1-year interim analysis. Bone 2001;28:310-15.
- Reid IR, Wattie DJ, Evans MC, et al. Continuous therapy with pamidronate, a potent bisphosphonate, in postmenopausal osteoporosis. J Clin Endocrinol Metab 1994;79:1595-9.
Resources
International Osteoporosis Foundation
W:www.osteofound.org
European Calcified Tissue Society
W:www.ectsoc.org
Forthcoming event
10–14 May 2002
IOF World Congress on Osteoporosis
Lisboa Congress Centre, Portugal
For more information contact:
IOF Congress Secretariat
T:+33 4 72 91 41 77
F:+33 4 72 36 90 52
E:[email protected]