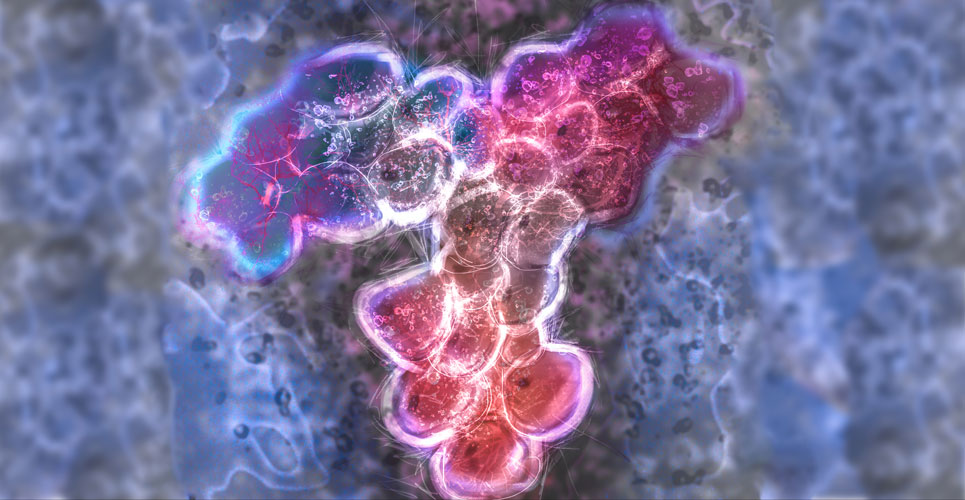
The two monoclonal antibodies, tocilizumab and sarilumab are directed against interleukin-6 (IL-6), which is released in response to infection and which stimulates inflammatory pathways. Interim analysis of the REMAP-CAP study suggest that both appear to benefit critically ill COVID-19 patients.
The randomised, embedded, multifactorial adaptive platform trial for community-acquired pneumonia (REMAP-CAP) is an on-going study that started in March 2020 and is designed to determine the best treatment strategy for patients with severe pneumonia in both pandemic and non-pandemic settings. The trial is designed with several different domains covering a therapeutic area, for example, antiviral therapy, and each domain contain two or more interventions and eligible patients assigned to one intervention in each domain. Patients who are critically ill with COVID-19, i.e., those in an intensive care unit receiving respiratory or cardiovascular organ support are eligible for inclusion in the COVID-10 immune modulation therapy domain. This latter domain has five interventions: tocilizumab, sarilumab, anakinra (an interleukin-1 receptor antagonist), interferon beta-1a as well as a control arm (without immune modulation but representing standard care) and eligible patients are assigned to one of these arms. Tocilizumab is given at dose of 8mg/kg (to a maximum of 800mg) and administered as an infusion over 1 hour and repeated 12 – 24 hours at the discretion of the clinician. Sarilumab is given at a dose of 400mg (intravenously) only once. The primary outcome for the REMAP-CAP trial was respiratory and cardiovascular organ support-free days up to day 21. All hospital-related deaths are assigned the worse outcome (-1) and among survivors up to day 21, organ support-free days are calculated such that a higher number, indicates a faster recovery. Earlier work has determined that a difference of 1.5 days can be considered as the minimal clinically important difference.
Findings
The interim analysis included 895 patients randomised to the immune modulation therapy domain, 366 to tocilizumab, 48 to sarilumab, 412 to control and 69 to other interventions within the domain. All patients were receiving either supplemental oxygen, or invasive mechanical ventilation. The median organ support-free days were 10 (tocilizumab), 11 (sarilumab) and 0 (control patients) which gave adjusted odds ratios of 1.64 (tocilizumab) and 1.76 (sarilumab), both of which were statistically significant. Furthermore, hospital mortality was 28% for tocilizumab and 22.2% for sarilumab compared to 35.8% for those assigned to control. The authors concluded that both treatments improved outcomes for critically ill patients and reduced mortality from infection with COVID-19.
Citation
The REMAP-CAP investigators. Interleukin-6 receptor antagonists in critically ill patients with COVID-19- preliminary report. medRxiv preprint doi.org/10.1101/2021.01.07.21249390