Niclosamide has been found to be no better than use of placebo at oropharyngeal clearance of COVID-19 viral particles after three days
The use of niclosamide to reduce COVID-19 viral shedding and symptoms appears to be no better than placebo according to the results of a randomised control trial by researchers from Tufts Clinical and Translational Science Institute, Tufts University, Boston, US.
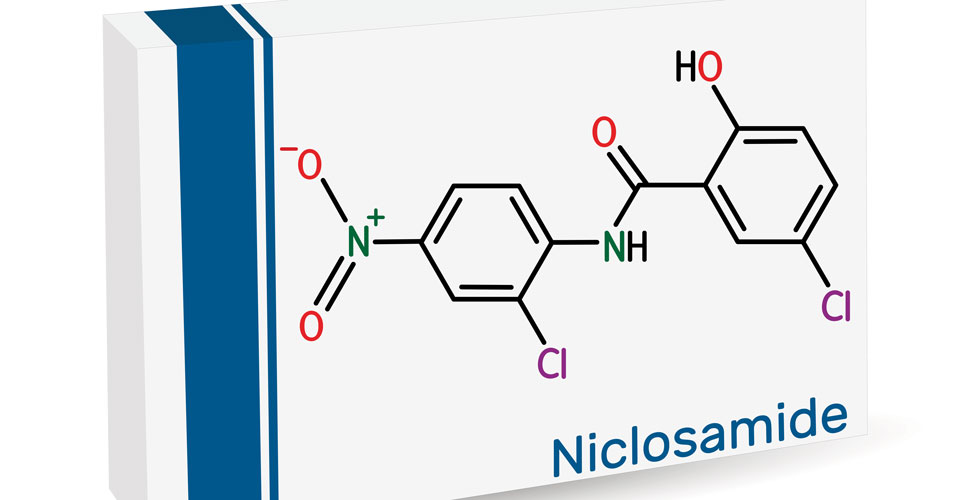
Niclosamide was developed and marketed as an oral anti-helminthic drug used to treat parasitic infections although interestingly, a 2004 study found that the drug was able to inhibit SARS-CoV replication. With much effort directed at re-purposing drugs during the COVID-19 pandemic, niclosamide has also been shown to possess anti-viral activity against COVID-19 and some of its variants. With the potential to halts COVID-19 viral entry into cells by altering endosomal pH and prevents viral replication, the authors of the present study, hypothesised that by reducing viral replication, niclosamide could attenuate COVID-19 symptoms among infected individuals.
The US team recruited patients with a positive PCR test for COVID-19 and who were either asymptomatic or had mild to moderate symptoms but excluded those with more severe disease who required hospitalisation. In addition to the provision of standard care, participants were randomised 1:1 to receive niclosamide 2 g orally for 7 days or a matching placebo with both participants and investigators blinded to participant’s assignment. The primary efficacy endpoint was the proportion of patients with viral clearance in respiratory samples acquired after 3 days, although sampling was performed on days 1, 3, 7, 10 and 14. A secondary outcome was the proportion of patients with faecal viral clearance after 14 days. They also examined the safety of the drug in terms of the incidence of adverse effects.
Niclosamide and COVID-19 viral clearance
A total of 67 participants with a mean age of 36.3 years (61.2% male) were enrolled and randomised to niclosamide (33) or placebo.
The primary outcome of oropharyngeal clearance after 3 days occurred in 66.7% of those assigned to niclosamide and 55.9% of those given placebo and this difference was not significant (p = 0.37). Among patients who were symptomatic with COVID-19, the mean duration of symptoms was 12 days (95% CI 8.82 – 15.2) compared to 14.61 (95% CI 11.25 – 17.96) in the placebo group which was non-significant.
For the secondary outcome of faecal clearance, there was also a non-significant difference (6.12 vs 5.77 days, niclosamide vs placebo). In subgroup analysis, participants who were considered to to overweight or obese (i.e., with a body mass index > 25), the mean time to symptom resolution was 11.57 days and 16.46 days, niclosamide and placebo respectively, which was also not significantly different.
In terms of safety, niclosamide was well-tolerated and the most commonly reported adverse events in the placebo and niclosamide groups were statistically similar and included headaches (32.4% vs 21.2%, treatment vs placebo, p = 0.31) and cough (23.5% vs 21.2%, treatment vs placebo, p = 0.82).
In terms of safety, niclosamide was well-tolerated and the most commonly reported adverse events in the placebo and niclosamide groups were statistically similar and included headaches (32.4% vs 21.2%, treatment vs placebo, p = 0.31) and cough (23.5% vs 21.2%, treatment vs placebo, p = 0.82).
Citation
Cairns DM et al. Efficacy of Niclosamide vs Placebo in SARS-CoV-2 Respiratory Viral Clearance, Viral Shedding, and Duration of Symptoms Among Patients With Mild to Moderate COVID-19: A Phase 2 Randomized Clinical Trial JAMA Netw Open 2022