James J Ferguson
MD FACC
Associate Director of Cardiology Research
Texas Heart Institute
Houston, Texas
USA
Currently, GPIIb/IIIa antagonists are felt to greatly reduce ischaemic complications associated with percutaneous coronary interventions (PCIs). They also appear to provide a more substantial benefit in the higher-risk population of patients with acute coronary syndrome (ACS). In short, the greater the risk, the greater the potential benefit.(1–3) From a physiological standpoint this makes good sense, because the platelet aggregation process that is so specifically inhibited by the GPIIb/IIIa antagonists has a major impact during the active thrombotic phase.
GPIIb/IIIa antagonists used in conjunction with coronary stenting
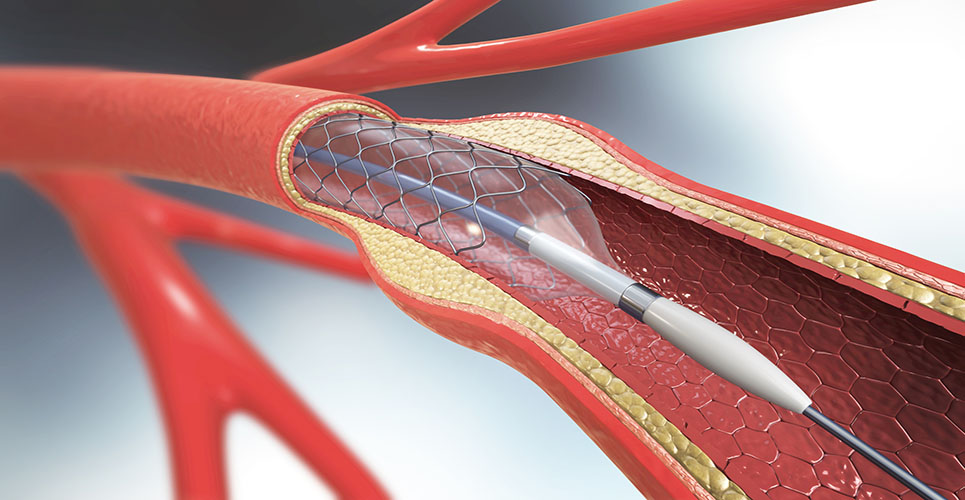
The beneficial effect on mortality rates of using one of the GPIIb/IIIa antagonists, abciximab, in combination with coronary stenting has been reinforced by data from the recent Evaluation of Platelet IIb/IIIa Inhibitor for Stenting Trial (EPISTENT),(4) and by a meta-analysis of the GPIIb/IIIa antagonist studies.(5) So far there are few specific data relating to the use of GPIIb/IIIa antagonists for PCI in patients with ACS, other than the data from the earlier GPIIb/IIIa trials, such as the Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis (RESTORE), which did not include the use of stents.(6) The only current long-term IIb/IIIa stent data are from EPISTENT, which included both low-risk and non-low-risk patients.
The recent European/Australian Stroke Prevention in Reversible Ischaemia Trial (ESPRIT) of eptifibatide, a small molecule IIb/IIIa antagonist, did not include higher-risk patients or patients who would otherwise receive a GPIIb/IIIa antagonist. The 30-day and 6-month results showed that eptifibatide produced a significant reduction in the composite endpoint of death, myocardial infarction (MI) or urgent revascularisation, although longer-term data are not yet available.(7)
Additional recent data are available from the Abciximab Before Direct Angioplasty and Stenting in Acute Myocardial Infarction Regarding Acute and Long-Term Follow-Up (ADMIRAL) study(8) and a study by Neumann et al.(9) Both of these studies utilised abciximab as an adjunct to coronary stenting for acute MI and showed substantial clinical benefit associated with its use. Some of this benefit probably arises from a significant improvement in microvascular perfusion a number of days out from the infarct. In the ADMIRAL trial, this was manifested in higher Thrombolysis in Myocardial Infarction (TIMI) flow scores at follow-up angiography; in the Neumann study, this was manifested as a trend towards higher coronary flow and coronary flow reserve upon pharmacological stimulation at 14 days (using Doppler velocity measurements).
The results of the CADILLAC study – conflicting evidence?
Data from the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) were presented recently.(10) CADILLAC was a factorially designed trial examining the effects of stenting versus balloon angioplasty and abciximab versus placebo in patients undergoing primary intervention for acute MI. In contrast to the ADMIRAL and Neumann studies, CADILLAC suggested that the addition of abciximab to coronary stenting provided no significant incremental benefit over stenting alone in
6-month major adverse cardiac events.(10) However, in retrospect, there was substantial benefit of abciximab in reducing ischaemic endpoints (not target vessel revascularisation), there were a relatively high number of patients with patent vessels at the time of the procedure, the overall event rates were relatively low, and the factorial design may have created some selection bias towards the inclusion of lower-risk patients. Again, these data are fairly recent, and final publication of the results is awaited.

What is needed in the future?
Further documentation and evaluation of the CADILLAC results are needed, as is an opportunity to try to resolve some of the apparently disparate results.
It is also important to address a fundamental “disconnect” that exists in the marketplace. On the one hand, abciximab is generally acknowledged as probably the most potent of the GPIIb/IIIa antagonists and perhaps the preferred agent in higher-risk circumstances.(11) However, in real-world practice, patients with ACS are also given “upstream” therapy initiated with the small-molecule-competitive GPIIb/IIIa antagonist (eptifibatide or tirofiban). Hence, higher-risk patients, in whom one might want a more potent form of therapy, may be getting something else. Is this right or wrong? At this point, the answer to this question is just not known. In the recent Do Tirofiban and ReoPro Give Similar Efficacy Outcomes Trial (TARGET), a direct comparison of abciximab and tirofiban, abciximab was shown to be significantly superior to tirofiban.(12) The majority of this benefit appeared to reside in patients with ACS. However, this was not a clearly prescribed subgroup. Admittedly, TARGET is not a pure ACS trial, but it is the first direct head-to-head comparison of two IIb/IIIa antagonists.
The recently published results of the Treat Angina with Aggrastat and Determine Cost of Therapy with an Invasive or Conservative Strategy (TACTICS-TIMI 18) trial (in which all patients received aspirin, heparin and tirofiban, and were randomised to an invasive versus a conservative strategy) further confounds issues. In this trial, the invasive strategy was found to be significantly superior. However, all patients received tirofiban.
The higher the risk, the higher the potential benefit of a more effective therapy, and the greater the potential cost-benefit of a more expensive therapy. As yet, no directly comparative cost-efficacy data are available, but this will hopefully become available from TARGET.
Why use GPIIb/IIIa antagonists at all?
Given the importance of platelets in acute thrombosis, GPIIb/IIIa antagonists may substantially improve our ability to treat and limit thrombus formation. As mentioned above, the GPIIb/IIIa antagonists will be most beneficial in acutely thrombotic circumstances. For a while, they were being broadly and enthusiastically used in ACS. Now, following the results of the TARGET, TACTICS, ADMIRAL and CADILLAC trials, and given the realistic cost-constraints that exist in the modern practice of medicine, it may be necessary to be a bit more circumspect in their application. Nevertheless, current data indicate that GPIIb/IIIa antagonists are a major therapeutic advance and appear to synergise well with other new forms of therapy. They are part of the standard treatment for coronary intervention, particularly for patients with ACS.
References
- The PURSUIT Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998;339: 436-43.
- The PRISM Study Investigators. A comparison of aspirin plus tirofiban with aspirin plus heparin for unstable angina. N Engl J Med 1998;338:1498-505.
- The PRISM-PLUS Study Investigators. Inhibition of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non-Q-wave myocardial infarction. N Engl J Med 1998;338:1488-97.
- The EPISTENT Investigators. Randomised placebo- controlled and balloon-angioplasty – controlled trial to assess safety of coronary stenting with use of platelet glycoprotein-IIb/IIIa blockade. Lancet 1998;352:87- 92.
- Kong DF, Califf RM, Miller DP, et al. Clinical outcomes of therapeutic agents that block the platelet glycoprotein IIb/IIIa integrin in ischemic heart disease. Circulation 1998;98:2829-35.
- The RESTORE Investigators. Effects of platelet glycoprotein IIb/IIIa blockade with tirofiban on adverse cardiac events in patients with unstable angina or acute myocardial infarction undergoing coronary angioplasty. Circulation 1997;96:1445-53.
- The ESPRIT Study Investigators. Novel dosing regimen of eptifibatide in planned coronary stent implantation: a randomised, placebo-controlled trial. Lancet 2000; 356:2037-44.
- Ecollan P, Montalescot G, De La Coussaye JE, et al. Poster; 72nd Scientific Sessions of the American Heart Association, Atlanta, GA, USA, November 1999.
- Neumann FJ, Kastrati A, Schmitt C, et al. Effect of glycoprotein IIb/IIIa receptor blockade on recovery of coronary flow and left ventricular function after the placement of coronary-artery stents in acute myocardial infarction. Circulation 1998;98:2695-701.
- Stone G. Oral presentation; 72nd Scientific Sessions of the American Heart Association, Atlanta, GA, USA, November 1999.
- Vanscoy GJ, Rihn TL. GPIIb/IIIa receptor inhibitors: clinical and cost considerations in acute coronary syndromes. Formulary 1999;34:500-12.
- Alexander W. TARGET: abciximab reduces need for percutaneous coronary intervention. Available from URL: www.cardiologytoday.com/200101/target.asp