This clinical guideline offers evidence-based advice on the diagnosis and management of chronic hepatitis B in children, young people and adults.
It updates and replaces recommendations 1.2 to 1.4 in Adefovir dipivoxil and peginterferon alfa-2a for the treatment of chronic hepatitis B (NICE technology appraisal guidance 96) on the use of adefovir dipivoxil for treating chronic hepatitis B.
This clinical guideline offers evidence-based advice on the diagnosis and management of chronic hepatitis B in children, young people and adults.
It updates and replaces recommendations 1.2 to 1.4 in Adefovir dipivoxil and peginterferon alfa-2a for the treatment of chronic hepatitis B (NICE technology appraisal guidance 96) on the use of adefovir dipivoxil for treating chronic hepatitis B.
NICE technology appraisal guidance 153, 154, 173 and recommendation 1.1 of NICE technology appraisal guidance 96 have been incorporated into this guideline and remain extant.
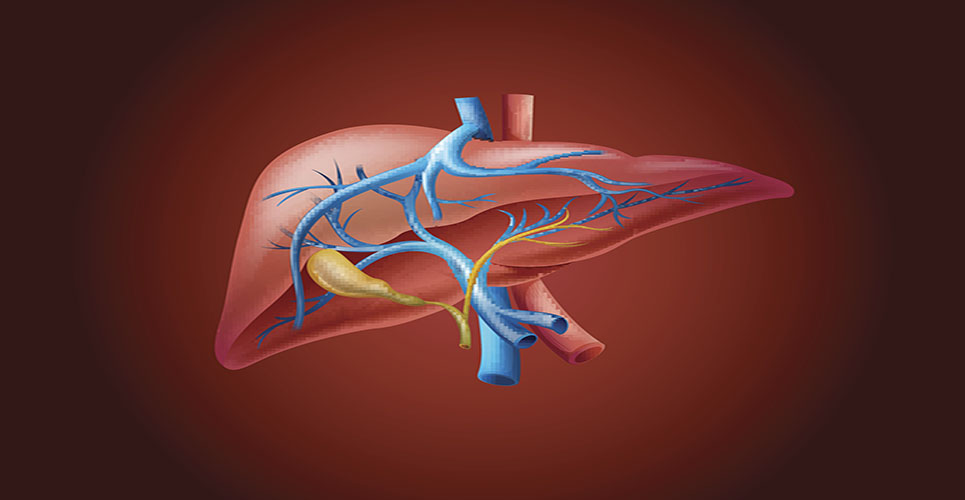
Chronic hepatitis B describes a spectrum of disease usually characterised by the presence of detectable hepatitis B surface antigen (HBsAg) in the blood or serum for longer than 6 months. In some people, chronic hepatitis B is inactive and does not present significant health problems, but others may progress to liver fibrosis, cirrhosis and hepatocellular carcinoma (HCC). The progression of liver disease is associated with hepatitis B virus (HBV) DNA levels in the blood.
Without antiviral treatment, the 5-year cumulative incidence of cirrhosis ranges from 8 to 20%. People with cirrhosis face a significant risk of decompensated liver disease if they remain untreated. Five-year survival rates among people with untreated decompensated cirrhosis can be as low as 15%.
Chronic hepatitis B can be divided into e antigen- (HBeAg) positive or HBeAg-negative disease based on the presence or absence of e antigen. The presence of HBeAg is typically associated with higher rates of viral replication and therefore increased infectivity.
The goal of treatment for chronic hepatitis B is to prevent cirrhosis, HCC and liver failure. In clinical practice surrogate markers are used to monitor progression of disease and treatment response, and include normalisation of serum alanine aminotransferase (ALT) levels, decrease in inflammation scores with no worsening or improvement in fibrosis on liver biopsies, suppression of serum HBV DNA to undetectable levels, loss of HBeAg and seroconversion to HBe antibody (anti-HBe), and loss of HBsAg and seroconversion to HBs antibody (anti-HBs).
Antiviral therapy suppresses HBV replication and decreases hepatic inflammation and fibrosis, thereby reducing the likelihood of serious clinical disease. Since the introduction of effective treatment in the form of interferon alfa, several nucleoside and nucleotide analogues are now approved for use in adults with chronic hepatitis B, together with a pegylated form of interferon alfa. With multiple treatment options that are efficacious and safe, the key questions are which patients need immediate treatment and what sequence and combination of drug regimens should be used, and which patients can be monitored and delay treatment.
In this guideline we cover the following:
- information needs of people with chronic hepatitis B and their carers
- where children, young people and adults with chronic hepatitis B should be assessed
- assessment of liver disease, including the use of non-invasive tests and genotype testing
- criteria for offering antiviral treatment
- the efficacy, safety and cost effectiveness of currently available treatments
- selection of first-line therapy
- management of treatment failure or drug resistance
- whether there is a role for combination therapy
- when it is possible to stop treatment
- managing the care of pregnant and breastfeeding women and prevention of vertical transmission
- prophylactic treatment during immunosuppressive therapy
- monitoring for treatment response, severity of fibrosis and development of HCC.
The spontaneous mutation rate of HBV DNA is high. Exposure of HBV to nucleoside or nucleotide analogues selects for mutations in the polymerase gene that confer resistance or decreased susceptibility to the drugs. The relative risk of drug resistance must be taken into account when considering treatment with nucleoside or nucleotide analogues, including the level of cross resistance between different agents.
Figure 1 depicts the natural history of chronic HBV infection. The immune-tolerance phase is seen in HBeAg-positive disease and is characterised by high levels of HBV replication with normal ALT levels and limited liver necroinflammation. Because there is minimal immune response to the virus it is unusual for spontaneous HBeAg loss to occur. This phase is commonly seen in children. It is followed by an immune-clearance or immune-reactive phase in which the immune system recognises and starts to clear the virus. ALT levels are typically elevated or fluctuating, and there is a higher risk of liver fibrosis. This tends to be the initial phase in people infected with HBV as adults. It lasts from weeks to years and ends with HBeAg seroconversion.
With the loss of HBeAg the person may enter an immune-control phase with very low or undetectable HBV DNA levels, normal ALT and minimal fibrosis progression. However, some people may experience rising HBV DNA levels despite HBeAg negativity. This is caused by virions that do not express HBeAg because of genetic mutations. This immune-escape phase can lead to active necroinflammation and progression of fibrosis.
Substantial progress has been made in the treatment of chronic hepatitis B in the past decade but the appropriate time for starting treatment remains a topic of debate. Although currently available treatment is effective in suppressing HBV replication, it fails to eradicate the virus necessitating long treatment duration and perhaps lifelong treatment.
The guideline will assume that prescribers will use a drug’s summary of product characteristics to inform decisions made with individual patients.
This guideline recommends some drugs for indications for which they do not have a UK marketing authorisation at the date of publication, if there is good evidence to support that use. The prescriber should follow relevant professional guidance, taking full responsibility for the decision. The patient (or those with authority to give consent on their behalf) should provide informed consent, which should be documented.
See the General Medical Council’s Good practice in prescribing medicines – guidance for doctors for further information. Where recommendations have been made for the use of drugs outside their licensed indications (‘off-label use’), these drugs are marked with a footnote in the recommendations.