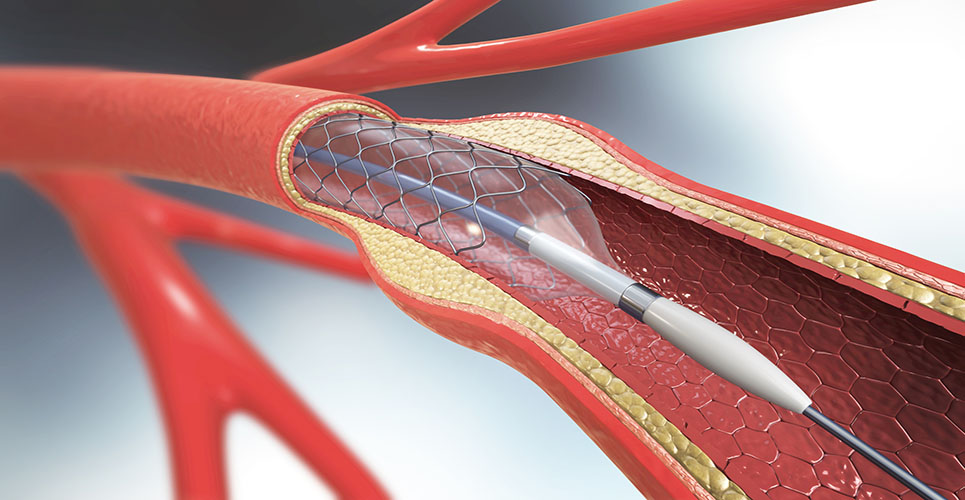
teaser
The generalised use of drug-eluting stents (DES) results in better outcomes than bare-metal stents (BMS), with fewer clinically-driven revascularisation procedures and similar rates of death and myocardial infarction (MI) at one year, according to a study published in the Journal of the American College of Cardiology.
Researchers evaluated data from patients in the National Heart, Lung, and Blood Institute Dynamic Registry enrolled in 2004 who received at least one DES (n = 1,460) and compared them with 1763 patients enrolled in the recruitment period immediately preceding the approval of DES (2001 to 2002) who received at least one BMS.
The following results were reported:
* At one year, cumulative death and MI was 7.6% in DES- and 8.7% in BMS-treated patients (adjusted hazard ratio [HR] 0.88, 95% confidence interval [CI] 0.68 to 1.15; p = 0.34);
* The one-year rate of target vessel revascularisation was 5.0% in DES and 9.2% in BMS patients (p < 0.001), and the risk of any repeat revascularisation by percutaneous coronary intervention or coronary bypass was lower in DES patients (adjusted HR 0.38, 95% CI 0.25 to 0.60; p < 0.001).
The authors also highlighted some of the following limitations to the study:
* Stent selection was not randomised and physician bias in choosing stent type could not be assessed, therefore DES patients were compared to those treated with BMS before availability of DES. The DES patients, however, may be more “selected” than the BMS patients;
* Routine angiographic follow-up was not a component of the study design. Therefore, the authors were unable to determine rates of in-stent restenosis or target lesion revascularisation.
* There were also lesions in both BMS and DES cohorts that were treated with balloon angioplasty alone, and some DES patients also received BMS, but the rates were low and these lesions were excluded from the target vessel revascularisation analysis;
* There were no long-term outcomes because the current analysis was limited to one-year follow-up.
American College of Cardiology