The important pharmacy-led #KnowYourDrops campaign was launched in Summer 2016 to promote and encourage eye drop compliance, provide support to patients, carers and staff regarding best eye drop techniques, and demonstrate a range of compliance aids to patients at Moorfields Eye Hospital NHS Foundation Trust.
Poor existing patient support for eye drop compliance
The important pharmacy-led #KnowYourDrops campaign was launched in Summer 2016 to promote and encourage eye drop compliance, provide support to patients, carers and staff regarding best eye drop techniques, and demonstrate a range of compliance aids to patients at Moorfields Eye Hospital NHS Foundation Trust.
Poor existing patient support for eye drop compliance
Support for correct eye drop technique and compliance aids is often overlooked outside specialist ophthalmic units compared with other specialist medicines, for example, inhalers, where dedicated time is usually spent assessing, reviewing and continually supporting technique. Eye drop technique support is also essential, because treatment does not always improve sight (often a motivator to use drops correctly) but can prevent disease progression, such as in glaucoma. Up to 50% of glaucoma patients are not compliant with treatment1 and given the consequences of treatment failure, it is vital to consider reasons for non-adherence to help overcome these.
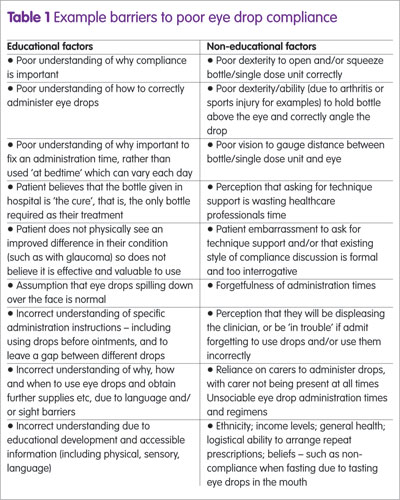
With there being various barriers to good compliance (Table 1), this can lead to poor clinical outcomes, unnecessary polypharmacy and/or financial losses.
All Moorfields, patients are reviewed and counselled on eye drop compliance and techniques, and it is strongly recognised that continual support assessment is vital to aid consistent compliance as a multidisciplinary team approach. The Public Health Outcomes Framework also supports this, describing how health campaigns, building eye care pathways around the needs and experiences of patients, and improving concordance are essential to prevent sight loss. Furthermore, the National Institute for Health and Care Excellence (NICE) specifically recommends supporting eye drop compliance.2
Together with the clinical team, pharmacy decided to raise awareness of compliance and eye drop techniques, offer enhanced support to patients, carers and staff in order to reduce barriers for good compliance, and therefore treatment failures, through the #knowyourdrops campaign. The International Glaucoma Association (IGA) greatly supported this initiative since eye drop compliance, especially for glaucoma, is essential for achieving effective outcomes.2
Campaign format
#knowyourdrops is a one-day advertised event at each Moorfields site, of which there are 32 spread across London, with advice and information on the Trust’s website and Twitter – including a useful online video and an opportunity to live-tweet compliance-related questions.
Glaucoma clinics were initially chosen, due to patients generally being on multiple long-term drops. Engagement with local clinical commissioning groups, GPs, community partners and local eye networks through the clinic liaison officers helped to raise awareness and invitation.
The lead Consultant opens the session by speaking about compliance and eye drop techniques to all patients/carers, inviting everyone to talk to us for a review and advice. We integrate with the clinic team to deliver a specialist pharmacist- led consultation by assessing patients to achieve best techniques, raising awareness of compliance, and demonstrating compliance aids. We have an eye-catching patient-facing stand with information, videos and compliance aids. We deliver interactive lunchtime workshops to all staff, which includes best techniques, patient assessments, and compliance aids.
Patient/carer case studies
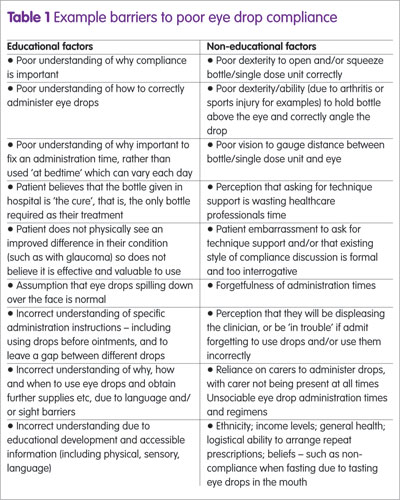
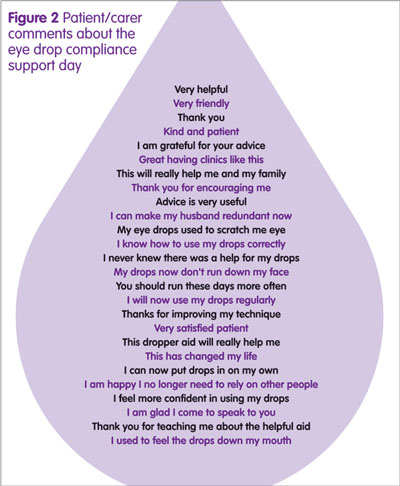
Numerous cases of improved medical care and quality of life (QoL) for patients as well as carers were achieved, all varying in nature and addressing many compliance barriers (Table 2).
Patient/carer feedback
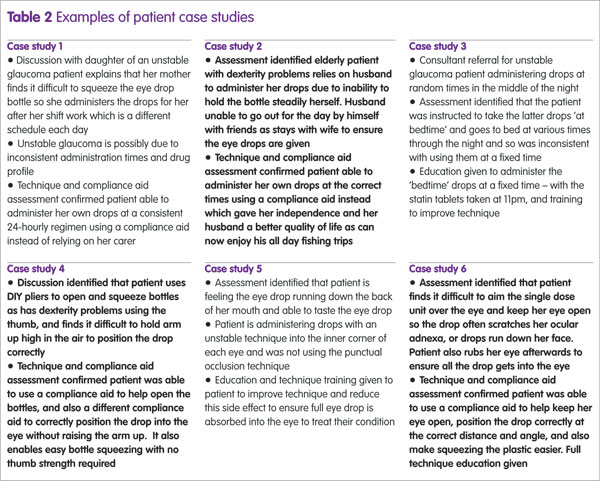
The presence of the campaign team assessing and supporting patients’ compliance was well received in all clinics, with exclusively positive comments collected from patients and carers associated with improved care and QOL (Figure 2).
Technique improvement
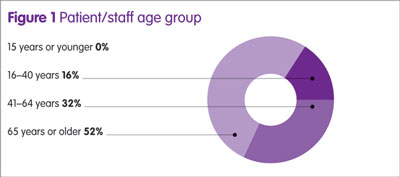
Patients/carers were invited to provide feedback about the support via a questionnaire (Table 3 and Figure 1). Data have so far been collected from five sites, with 44 feedback forms completed. All patients/carers (n=44) expressed that the eye drop compliance support was useful to help improve the way they delivered eye drops, and felt more confident in putting in eye drops than they did before. Over half of those providing feedback were over 65 years of age (n=23).
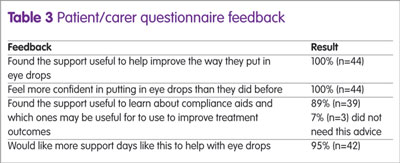
Compliance aid awareness
Almost all patients/carers (89%) said that they found the support day useful to learn about compliance aids and which ones may be useful to help improve their treatment outcomes.
Additional specialist pharmacist-led consultation sessions
Almost all patients/carers (95%) said that they would like more support days like this to help with eye drops.
Staff feedback
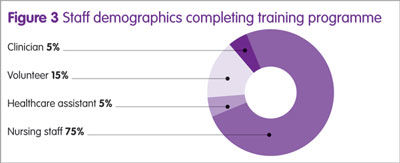
Feedback from staff was very positive about the #knowyourdrops team being present, and also about the staff education workshop. Differing staff groups attended the workshops, and 20 completed feedback questionnaires (Figure 3 and Table 4).
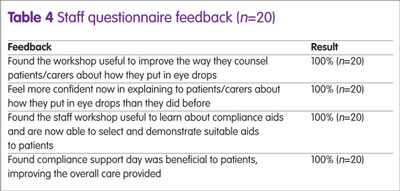
All staff said they felt the learning workshop had improved their skills and confidence to help patients’ compliance, and that they now knew how to assess and use the range of compliance aids. Positive comments received include:
- ‘An excellent resource for staff education and patients. It was highly informative, good to play around with the devices and talk as a group about barriers for patient’ (Senior Consultant).
- ‘Please attend the outpatient clinic to find out who needs assistance on a regular basis’ (Sister).
- ‘This awareness is good to help patients be aware of the available aids to facilitate eye drop compliance and easy application’ (Nurse).
- ‘Very helpful, understood more about drops today and will be able to keep my patients better from now on’ (Healthcare Assistant).
- ‘Now I have an increased knowledge of aids. Quite a lot of patients these days need aids so this is very helpful’ (Nurse).
Discussion
Treatment and care should take into account people’s needs and preferences,2 and as studies have found, there is not always a general relationship between medication adherence and the patients’ demographic data, clinical characteristics, or knowledge.3
Eye drops are not easy to administer, relative to oral dosing, including those given via multi-dose eye drop bottles where the inherent difficulties of delivering these medications have been reviewed in various studies.4,5 One study showed only 39% of patients with glaucoma administered the drops successfully.
With the numerous varied patient case studies already identified through this campaign, it is apparent that a patient-specific approach is required to optimise adherence behaviour to eye drops, for new and existing patients.
A patient-specific approach
To effectively break barriers to eye drop adherence, support must encompass a varied educational approach specific to each individual patient. It is simply inadequate to provide basic administration time counselling with a patient information leaflet, a poor quality demonstration and acceptance from the patient that they follow the correct technique after leaving the pharmacy counter. Frequently, new and existing patients realised that they were not putting drops in correctly, and benefitted from a tailored educational pharmacist-led consultation session.
Assessing technique, identifying weaknesses, physical demonstrations and practicing, watching videos, worded and pictorial diagrams/leaflets, large font, translation services, speaking with other patients, and trying different devices with their bottles were all methods used. In addition, the patient-specific approach puts patients/carers at ease to engage in interactive conversations about compliance issues, which had often not yet been identified during their clinical pathway.
Repeated demonstrations also helped overcome any educational barriers and establish correct understanding, because single sessions have shown not to be as effective. According to one study, a single educational session on the proper use of topical drops was shown to improve the successful instillation of eye drops, however it did not determine whether patients retain the improved instillation technique for long-term or if the intervention only results in a short-term improvement.6
Furthermore, ensuring that patients know why, how and when to use drops, and provision of information about their condition, consequences of not using the medications properly, and the adverse effects of the medication can result in low adherence in glaucoma.7
Improved QoL for patients and carers
In many cases, the relatively simple intervention of spending 10–15 minutes to assess technique and encourage open and honest interactive discussion about compliance has not only helped improved clinical outcomes, but improved QOL – often providing feelings of independence, confidence, self-satisfaction, calmness and dignity.
According to one study, 17% of patients relied on another person to administer the drops,4 where poor manual dexterity and reduced vision often worsened the administration problems. The campaign hopes to raise healthcare professionals’ awareness that it is not always just the patient who benefits as it is often the carer, through lessening the burden and constraints of family members being relied upon multiple times a day to administer eye drops.
Role of the pharmacist
This campaign highlights that pharmacists must recognise that medicines optimisation in ophthalmology is often an overlooked area requiring professional awareness, skills and knowledge to provide better support across all patient groups. Most of the population will use eye drops at some stage in their lives and it is often assumed that basic counselling about drop frequency and a quick check that patients know how to use eye drops is sufficient for all. However, with 50% of all glaucoma patients being non-compliant with treatment1 and that 10% of UK blindness registrations are attributable to glaucoma,2 it is clear that this is an area where pharmacists can help make a positive difference. With glaucoma being the second leading cause of blindness globally,8 it has been stated that the assessment of a patient’s ability to instil eye drops correctly should be a routine part of the glaucoma examination. This needs to also be an integral part of each pharmacist counselling session.
Studies have shown that regular monitoring can help to ensure that the information has been retained by the patient.6 Pharmacists are ideally placed to improve eye drop compliance within the hospital as well as the community setting. However, few are actively providing this role. According to one study, 63% of patients were given advice about instillation technique, of which 5.3% received this by a hospital pharmacist, and 2% from a community pharmacist.
Time- and cost-savings
Several patients use excessive drops unnecessarily purely due to poor administration techniques, which adds to the burdens of repeat prescribing and national medication costs. By better supporting ophthalmic adherence, this not only improves treatment outcomes and QoL, but also helps to reduce pressures across the National Health Service by saving time and money.
Conclusions
This campaign marks an important landmark to help raise awareness of the importance of eye drop adherence support, and the weaknesses in current support provision. It is reasonable to note that there is often a lack of consideration of the need and subsequent benefits to care and QoL of both patient and carer. In addition, there is a potential lack of understanding, knowledge and skills to provide this necessary care among the profession.
In conclusion, an important part of poor adherence is an incorrect dosing technique,6 and healthcare professionals can reduce both educational and non-educational potential barriers to ophthalmic non-adherence for all patients as shown via this campaign. The #knowyourdrops eye drop compliance campaign helps achieve medicines optimisation in ophthalmology, and will therefore be fully integrated and rolled out to all areas regularly to all patients Trust-wide in 2017.
Key points
- Successful ophthalmic treatment relies on effective drug administration and all patients, regardless of previous eye drop therapy or length of treatment, benefit from an assessment of correct technique and potential barriers to achieve maximum therapeutic benefit.
- More than50% patients with glaucoma, an asymptomatic disease and leading cause of sight-loss, are non-compliant with using eye drops.
- Educating and engaging patients and carers about why, how and when to use their eye drops is essential to support medicines optimisation, all of which can be delivered by the pharmacy team as well as by clinicians and nursing staff.
- Support for eye drop compliance not only supports medicines optimisation but often significantly improves quality of life for patients and carers by, for examples, improving confidence, providing patient independence, improving patient experience and personal management of their condition, reducing reliance of carers to administer drops, and alleviating any stresses and operational burdens associated with using carers.
- Pharmacists can support the clinical team by reviewing patients at the initial stages of therapy along the patient treatment pathway, and also by providing continuous support throughout the treatment course. Routine counselling of repeat eye drops is a valuable opportunity to check technique and offer advice to improve this, and to ensure maximum benefit from treatment.
References
1 Johnson MRD et al. A review of evidence to evaluate effectiveness of intervention strategies to address inequalities in eye health care. RNIB and De Montfort University. www.rnib.org.uk/knowledge-and-research-hub/research-reports/prevention-sight-loss/intervention-strategies (accessed July 2017).
2 National Institute for Health and Care Excellence. Glaucoma: diagnosis and management. NICE clinical guideline 85. www.nice.org.uk/CG85 (accessed July 2017).
3 Welge-Lussen U et al. Assessing the adherence behaviour of glaucoma patients to topical eye drops. Patient Prefer Adherence 2015;9:17–23.
4 Hennessy AL et al. A video study of drop instillation in both glaucoma and retina patients with visual impairment. Am J Ophthalmol 2011;152(6):982–8.
5 Marston MV. Compliance with medical regimens: a review of the literature. Nurs Res 1970;19(4):312–23.
6 Lazcano-Gomez G et al. Video-graphic assessment of glaucoma drop instillation. J Curr Glaucoma Pract 2015;9(2):47–50.
7 Friedman DS et al. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology 2008;115(8):1320–7.
8 World Health Organization. Bull World Health Organization 2004;82(11):811–90.