teaser
Colin A Morton
MB ChB FRCP(UK) MD
Consultant Dermatologist
Department of Dermatology
Falkirk Royal Infirmary
Falkirk
UK
E:[email protected]
Systemic photosensitisation and endoscopic light delivery have permitted the treatment of many hollow organ tumours by photodynamic therapy (PDT), including those in the oesophagus, stomach, bronchus and bladder, curing early superficial disease and palliating late disease.(1) Several countries now have approved systemic PDT for these indications. Ease of light delivery to the skin makes PDT an attractive potential therapy for dermatology. Moreover, the development of topically active agents for PDT avoids the generalised photosensitivity that follows systemic photosensitiser use. Evidence-based guidelines indicate that, in dermatology, topical PDT is effective in actinic keratoses on the face and scalp, Bowen’s disease (squamous cell carcinoma in situ) and superficial basal cell carcinomas (BCC), with potential in nodular BCC.(2)
Topical PDT moved from research to clinic in November 1999 with FDA approval of PDT using a 5-aminolaevulinic acid preparation, Levulan Kerastick‚ and Blu-U light (DUSA, USA) for the treatment of actinic keratoses. In June 2001 the methyl ester of 5-ALA, MAL (Metvix; PhotoCure, Norway, and Galderma, France), was approved in Sweden for topical PDT of nonhyperkeratotic actinic keratoses of the face and scalp and for basal cell carcinomas unsuitable for conventional therapy. This approval of Metvix has now been extended to many European countries, including the UK, and to Australia, with approvals currently awaited in the USA.
Topical PDT offers the potential of a practical nonsurgical outpatient office therapy. Against the continued rise in incidence of cutaneous malignancy and ageing population profiles in most parts of the world, developing safe, effective and patient-friendly therapies is of great importance. PDT may prove advantageous where size, site or number of lesions limits the efficacy and/or acceptability of conventional therapies.(3) Topical PDT studies consistently report a superiority of the cosmetic outcome, with minimal or no scarring, compared with standard therapies: cryotherapy, topical 5-fluorouracil and surgery.
Topical PDT – method of action
5-aminolaevulinic acid (5-ALA) is a precursor in the haem biosynthesis pathway, in which the endogenous photosensitiser protoporphyrin IX (PpIX) is formed that binds with iron to form haem. Exogenous administration of 5-ALA or MAL increases the intracellular concentration of PpIX to therapeutically useful concentrations, although it is metabolised within 48 hours, avoiding prolonged phototoxicity.(4) Methyl-ALA, MAL, appears to have greater tumour selectivity, with three-hour application on a tumour surface inducing porphyrin formation throughout the depth of basal cell carcinomas up to 2mm thick.(5)
When a photosensitiser absorbs light, it is converted from a stable ground state to a short-lived singlet state that may undergo conversion to a longer-lived excited triplet state, the photoactive species responsible for the generation of cytotoxic products.(4) This may directly react with substrate by hydrogen atom or electron transfer to form radicals, or the triplet state can transfer its energy to oxygen directly to produce singlet oxygen, causing photo-oxidation and cell death. The complete process takes place in a timescale of microseconds and will occur close to the site of radical generation, with inhibition of mitochondrial enzymes likely to be the key event in ALA/MAL-PDT cell death.
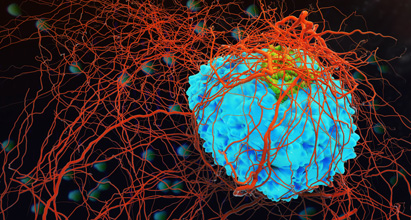
The predominant mechanism of action of topical PDT is presumed to be direct tumour cell kill, although in PDT with systemically administered photosensitisers an important contribution to tumour destruction is achieved via damage to the vascular supply. Immunologic effects may also contribute to the success of PDT, although their importance remains to be determined.
Light sources for topical PDT
PDT requires not only the uptake of photosensitiser by the target cells, but also the subsequent delivery of light of an appropriate wavelength and dose that will activate the absorbed agent. Lasers can be used, but coherence of light is not required, and xenon arc and incandescent filament lamps as well as light-emitting diodes (LEDs) are widely employed for the illumination of skin lesions.(6) The optimal part of the light spectrum required for PDT depends on the photosensitiser used and indication. Most lamps utilise the “red” 635nm absorption peak of PpIX in order to maximise tissue penetration. One fluorescent lamp is centred on the maximum but least-penetrating “blue” 410nm peak, which appears adequate for thin actinic keratoses.
PDT for actinic keratoses
Actinic keratoses are a widespread and common problem in dermatology, with a prevalence of around 24% in over-60-year-olds in the UK. Although the risk of progression to squamous cell carcinoma appears very low, it remains impossible to predict which actinic keratoses may progress to invasive squamous cell carcinoma. PDT may offer particular advantages over standard therapies as a relatively selective treatment with minimal or no scarring, with the potential that multiple lesions can be treated simultaneously.
Experience in the USA with Levulan as a formulation of 5-ALA in the treatment of actinic keratoses has used a specific nonlaser blue-light source, the Blu-U. A complete patient response rate of 72% for thin actinic keratoses on the face and scalp is reported.(7) The experience since 1990 using ALA-PDT in Europe has demonstrated high clearance rates, with a weighted clearance rate for facial actinic keratoses of 88%.(2)
A single treatment with MAL-PDT for thin and moderate- thickness actinic keratoses is equivalent to intense cryotherapy (75% and 81% respectively).(8) Statistically significant superiority of cosmetic outcome for PDT was demonstrated in this study.(9) In another study, two PDT treatments seven days apart were then compared with cryotherapy as performed in a dermatologist’s clinic.(9) The comparable clinical complete response rates were 91% for PDT and 68% for cryotherapy. PDT was demonstrated to be statistically superior to cryotherapy in efficacy and cosmetic outcome. Patient preference data accumulated during these studies indicate that patients have a preference for PDT over cryotherapy, 5-fluorouracil and surgery.
At the recent World Congress of Cancers of the Skin in Seville in May 2003, a multicentre intraindividual right–left arm comparison study demonstrated that MAL-PDT delays the occurrence of new skin lesions in organ transplant recipients. Although the study was performed over only one year, there was an increase in the mean time to a new lesion development following PDT of 9.6 months, in comparison with 6.8 months for control.(10) This suggests a potential role for PDT in cancer prevention as well as therapy.
PDT for squamous cell carcinoma in situ (Bowen’s disease)
Considerable research experience has been accumulated utilising topical ALA-PDT for Bowen’s disease, and results of a study using MAL are currently awaited. In a randomised comparison study of ALA-PDT with topical 5-fluorouracil in Bowen’s disease, PDT was shown to be significantly superior with disappointingly high recurrence rates in the 5-fluorouracil group. A complete clearance rate of 88% following PDT was compared with 66% for topical 5-fluorouracil group and the recurrence rate of 7% 12 months following PDT, compared with 27% after topical 5-fluorouracil.(11)
PDT for basal cell carcinoma
Many studies have reported the use of topical ALA-PDT in basal cell carcinomas, with a weighted complete clearance rate from 16 studies of superficial lesions of 87%.(2) Lesions estimated by pretreatment biopsy to be <2mm thick may respond especially well to topical PDT. Prior debulking curettage or treatment fractionation, with two treatments seven days apart, appear to improve response of nodular BCC to ALA-PDT, with response rates of 92% and 96% respectively.(12,13)
Large and multiple superficial BCCs may benefit particularly well from topical ALA-PDT.(3)
MAL-PDT has also been extensively studied for basal cell carcinoma. In one study of 120 patients a single cycle of MAL-PDT was undertaken in a randomised comparison study with cryotherapy.(14) Three-month complete response data demonstrated 97% of lesions cleared with MAL-PDT, compared with 95% of lesions with cryotherapy, and at one year the recurrence rate for MAL-PDT is 8%, in comparison with 16% with cryotherapy. Cosmetic outcome was superior following MAL-PDT over cryotherapy. A further study has compared MAL-PDT with excision surgery in primary nodular basal cell carcinoma. Impressive clearance rates at three months of 90% with MAL-PDT compared with 98% with surgery.(15) It is important to note that, in undertaking MAL-PDT in nodular basal cell carcinoma, protocols describe prior debulking of the central component before PDT. This is undertaken typically with a curette but is a subtotal preparation sparing the rim of the tumour and does not require local anaesthesia.
PDT – no pain, no gain?
Discomfort, often described as a burning, stinging sensation, is often reported during topical PDT and probably reflects local nerve stimulation/damage during PDT.(16) Most patients will tolerate topical PDT without anaesthesia/ analgesia with strategies to reduce pain available if required, topical/injected local anaesthetic or cooling fans. A comparison of ALA-PDT with MAL-PDT in healthy volunteers confirmed that MAL-PDT was significantly less painful.(17)
Immediately following PDT, erythema and oedema are common, with erosion, crust formation and healing over two to six weeks. Comparisons with cryotherapy, 5-fluorouracil and surgery indicate that PDT is well tolerated, with post-treatment ulceration or infection less common following PDT.(2)
PDT – where next?
Topical PDT for localised cutaneous T-cell lymphoma has been reported successful in several small case reports.(18) Many inflammatory dermatoses could benefit from PDT, with a recent comprehensive review by Ibbotson et al.(19) Most study activity has focused on the potential of PDT in psoriasis, acne and viral warts. Treatment protocols are likely to be quite different in these indications, with repeated PDT using low-dose, low-intensity light preferable to higher-dose skin cancer regimens. Much research work is still required to demonstrate whether PDT for inflammatory dermatoses can demonstrate superiority over existing therapies.
Summary
Topical PDT has demonstrated efficacy for the treatment of actinic keratoses, Bowen’s disease and basal cell carcinoma.
There are now licensed indications for topical PDT for thin/nonhyperkeratotic actinic keratoses on the face and scalp and for superficial and nodular basal cell carcinomas unsuitable for other therapy. Although not yet licensed, topical PDT appears a good option for Bowen’s disease. Large and multiple actinic keratoses, Bowen’s disease and basal cell carcinomas may also respond well and have benefits over certain standard therapies.
There appears to be clear cosmetic advantage to using PDT over current therapies. As a relatively selective treatment with minimal or no scarring that is noninvasive and can be undertaken in an out-patient setting, topical PDT represents a useful additional therapy option in nonmelanoma skin cancer management.
References
- Hopper C. Lancet Oncol 2000;1:212-9.
- Morton CA, Brown SB, Collins C, et al. Br J Dermatol 2002:146:552-67.
- Morton CA, Whitehurst C, McColl JH, et al. Arch Dermatol 2001;137:319-24.
- Henderson BW, Dougherty TJ. Photochem Photobiol 1992;55:145-57.
- Peng Q, Soler AM, Warloe T, et al. J Photochem Photobiol B – Biol 2001;62:140-5.
- Brancaleon L, Moseley H. Lasers Med Sci 2002;17:173-86.
- Ormrod D, Jarvis B. Am J Clin Dermatol 2000;1:133-9.
- Szeimies M, Karrer S, Radakovic-Fijan S, et al. J Am Acad Dermatol 2002;47:258-62.
- Freeman M, Vinciullo C, Francis D, et al. J Dermatol Treatment 2003;14:99-106.
- Wulf HC, Stender IM, Beard A, et al. Presented at the 9th World Congress on Cancers of the Skin, Seville, Spain; 7–10 May 2003.
- Salim A, Leman JA, McColl JH, et al. Br J Dermatol 2003;148:539-43.
- Thissen MR, Schroeter CA, Neumann HA. Br J Dermatol 2000;142:338-9.
- Haller JC, Cairnduff F, Slack G, et al. Br J Dermatol 2000;143:1270-74.
- Basset-Sequin N, Ibbotson S, Emtestam L, et al. J Eur Acad Dermatol Venereol 2001;15 Suppl 2:226.
- Rhodes LE, De Rie M, Enstrom Y, et al. Presented at the Annual Meeting of the American Academy of Dermatology, San Francisco, USA; 21–26 March 2003.
- Grapengiesser S, Gudmundsson F, Larko O, et al. Clin Exp Dermatol 2002;27:493-7.
- Wiegell S, Stender IM, Na R, Wulf HC. Arch Dermatol 2003;139:1173-7.
- Leman JA, Dick DC, Morton CA. Clin Exp Dermatol 2002;27:516-8.
- Ibbotson SH. Br J Dermatol 2002;146:178-88.