teaser
Zoledronic acid, a potent heterocyclic amino-bisphosphonate, has been shown to be effective in preventing fractures in patients with a previous history of hip fractures
Nuttan Tanna
MRPharmS DComP PhD
Pharmacist Consultant
Womens Health & Older
People
Womens Services
NW London Hospitals
NHS Trust
Harrow, London
UK
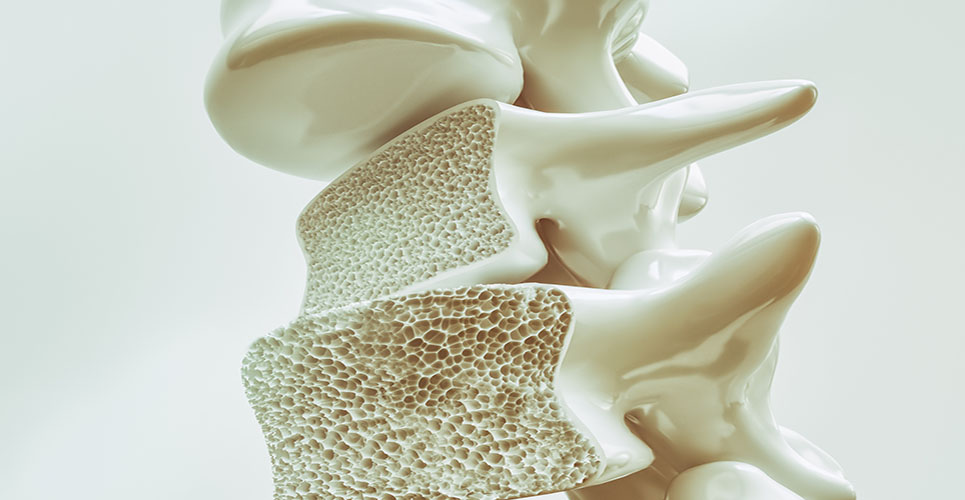
Bisphosphonates are analogues of pyrophosphate in which the labile P-O-P bond has been replaced with the more stable P-C-P bond. This bond is resistant to hydrolysis and enzymatic destruction. All the compounds in current use have the same basic structure and differ only in respect to the length and composition of the carbon side-chain. A “nitrogen” – containing amino side-chain makes the bisphosphonate much more potent in activity (Figure 1).
[[HPE.40]]
Zoledronic acid is a heterocyclic amino-bisphosphonate compound that has been available for some time for the treatment of complications of malignancy and for Paget’s disease. A 4 mg IV formulation is widely used to reduce skeletal events in patients with advanced cancer[1], and a 5 mg formulation, given as a single infusion, is an efficacious treatment for Paget’s disease[2]. The licence for zoledronic acid has recently been extended both in the EU and USA to include the treatment of osteoporosis in postmenopausal women at increased risk of fracture. For this indication, zoledronic acid is administered as a once-yearly intravenous infusion (Figure 2).
[[HPE.41]]
Bisphosphonates are antiresorptive agents, acting during the bone remodelling phase to decrease osteoclast activity and induce osteoclast apoptosis. This allows more time for secondary mineralisation to proceed to completion in the existing bone tissue mass, so increasing the mechanical resistance of bone to loading. The present evidence base for the bisphosphonates supports the use of short-duration therapy in high-risk individuals.[3,4] The optimum duration for bisphosphonate prescribing has not been established.[5-7] In this article the evidence base for zoledronic acid in postmenopausal osteoporosis and fracture prevention is reviewed.
Zoledronic acid randomised controlled studies
Two large multicentre randomised controlled trials compared the effects of annual infusions of zoledronic acid 5 mg with placebo on incidence of fracture.[8,9] The first trial targeted postmenopausal women with osteoporosis (dual-energy X-ray absorptiometry scan reporting T-score of –2.5 or less at the femoral neck, or a T-score of –1.5 or less with evidence of vertebral fractures),[8] whilst the second trial included patients, both men and postmenopausal women, with a prior history of hip fractures.[9]
In the double-blind HORIZON Pivotal Fracture Trial (PFT)[8], 7,765 women aged 65-89 (mean age 73 years) were randomised to two study arms. The first strata included patients not taking osteoporosis medicines, whereas the second strata allowed concomitant use of the following bone-sparing treatments: hormone replacement therapy, raloxifene, calcitonin, tibolone, tamoxifen, dehydroepiandrosterone, ipriflavone and medroxyprogesterone. It is worth noting that medroxyprogesterone acetate (MPA) is a progestogen that has glucocorticoid activity.[10] There is evidence that MPA causes loss of bone mineral density.[11,12] It is debatable therefore whether MPA can be considered to be a “bone-sparing” treatment.
Patients who had previously used bisphosphonates and met washout criteria were randomised to either strata. Exclusion criteria included any previous use of parathyroid hormone, sodium fluoride or strontium, anabolic steroids or growth hormone within the previous six months, and oral or intravenous systemic corticosteroids within the previous 12 months.
All patients received oral daily calcium and vitamin D. Primary outcome measures were morphometric vertebral fracture in those not taking osteoporosis medications at baseline and hip fracture in all patients. Three annual infusions of zoledronic acid (n = 3,889) resulted in an absolute risk reduction of morphometric vertebral fracture of 7.6%, with relative risk of 0.3 (95% CI 0.24-0.38).

The number of patients needed to treat costeffectively (NNT) was 13 over three years. There was decreased risk for incidence of hip fracture (1.4% vs 2.5% respectively; hazard ratio 0.59), giving an NNT of 91 over three years. In the group of patients taking concurrent osteoporosis treatment, the reduction in incidence of hip fracture was nonsignificant. Zoledronic acid was associated with a significant improvement in bone mineral density (BMD) and bone metabolism markers.
Limitations included not all randomised participants being included in the analyses and a lack of active comparator. Withdrawals, however, accounted for less than 1% of the randomised sample. Data to compare zoledronic acid efficacy for fracture prevention on a head-to-head basis with alendronate, the current advocated first-line treatment for osteoporosis in the UK are needed and could have major implications for clinical practice.[13,14]
Alendronate is given as an oral treatment, on a daily or weekly basis. Patients have to adhere to a strict routine for good medication taking to maximise bisphosphonate safety and efficacy. Alendronate, for example, can cause oesophageal ulcers, and bioavailability is severely affected if taken with other drugs or foods. Oral bisphosphonate treatments cause gastrointestinal side-effects that can limit good concordance with treatments.
Cost comparisons cannot support therapeutic equivalence but generally form the basis of recommendations within health economies. Currently, generic alendronate is less than a fifth of the price of zoledronic acid.
In the HORIZON Recurrent Fracture Trial (RFT), 2,127 patients aged 50 years or over were randomised to receive zoledronic acid (n = 1,065; mean age 74.5) or placebo within 90 days after surgical repair of a lowtrauma hip fracture.[9] All patients received supplemental oral vitamin D and calcium, including a pharmacologically higher loading oral or injectable dose if necessary. With a median follow up of 1.9 years, the findings reported included a reduction in the cumulative rate of new clinical fractures and improved survival.
The research group altered the primary outcome from the mean time to first fracture to the rate of new clinical fracture. A limitation to this study, the reason given for making this change, was that the overall rate of fracture within trial participants was low. There was a 35% risk reduction with zoledronic acid for new clinical fracture, with an NNT for new clinical fractures of 19 at 1.9 years (hazard ratio 0.65). This is the only RCT that has found any bone-sparing treatment to be effective in preventing fractures in patients with a previous history of hip fracture. The safety analysis reported 9.6% deaths in the zoledronic acid group, as compared with 13.3% in the placebo group, a significant reduction of 28% in deaths from any cause in the zoledronic acid group (p = 0.01).
Both the research team[9] and Compston[15] suggest that the reduction in risk of death was probably multifactorial and cannot be attributed only to zoledronic acid therapy. It is important to note that the RFT did not show any statistically significant reduction in the rate of hip fractures, which are the fractures of most clinical interest because they cause the highest morbidity and mortality.
McClung et al[16] reported findings from their study using intravenous zoledronic acid 5 mg in the treatment of postmenopausal women with low bone density previously treated with alendronate. In this double-blind, randomised controlled trial, 225 women aged 45-79 with osteopenia,[17] with T-scores equal to or less than 2 at the lumbar spine or femoral neck and who had already been on treatment with alendronate for at least a year, were randomised to one infusion of zoledronic acid or 52 weekly doses of oral 70 mg alendronate.
BMD increases were greater in women on alendronate, but there was no statistically significant difference between treatment groups in the percent change from baseline at month 12 in lumbar spine BMD. Bone turnover markers initially decreased in the zoledronic acid patient group and then increased above baseline values but remained within acceptable pre-menopausal range. In women switched from oral alendronate to zoledronic acid infusion the same effects on BMD and markers of bone turnover are maintained for at least a year. Patients in this study were asked about their treatment preferences, with 79% indicating a preference for the annual infusion.
In a smaller randomised, double-blind, doubledummy, multicentre 24-week trial, Saag and colleagues[15] evaluated the onset of action of a single infusion of zoledronic acid 5 mg compared with weekly oral alendronate 70 mg (n = 69 and 59 respectively) in postmenopausal women with low BMD (T-score equal to or less than 2 by DXA).[15] This was assessed by
reductions in urinary N-telopeptide of type 1 collagen (NTX), and other bone markers, including serum b-CTX levels and BSAP, a marker of bone formation. The significantly greater reduction in urine NTX levels at week 1 with zoledronic acid suggests a more rapid onset of effect than alendronate 70 mg once weekly. All markers were within the premenopausal range by the end of the study, with levels of serum b-CTX returning to the premenopausal levels by week 12. Current medical consensus is that further work is needed as the use and value of bone markers within routine clinical practice has not yet been established.
Risk management
In the HORIZON PFT,8 serious atrial fibrillation (AF) was reported in 1.3% of treated patients, as compared with 0.5% in the placebo group. AF occurred in most cases more than 30 days after the infusion. In the HORIZON RFT,9 the incidence of serious AF was similar in the zoledronic acid and placebo groups (1.1% and 1.3% respectively). Within both HORIZON trials,[8,9] the most common postdose symptoms seen up to three days after infusion were pyrexia and myalgia, with the PFT8 also reporting influenza-like symptoms, headache and arthralgia, and the RFT[9] reporting bone and musculoskeletal pain in addition. Two cases of osteonecrosis of the jaw, one in each group, were reported from the PFT,[8] but none was noted in the RFT9. No adverse affect on fracture healing or renal safety was noted in either study.
Osteomalacia must be corrected for prior to bisphosphonate therapy,[13,14] and so all patients given zoledronic acid need to have adequate calcium and vitamin D intake or will require additional supplementation. Zoledronic acid is given as a slow intravenous infusion over 15 minutes, and patients should be appropriately hydrated prior to administration. This would be
particularly important for the elderly and for patients on diuretic treatment.
Summary
Zoledronic acid is a potent amino-bisphosphonate for use for postmenopausal osteoporosis with risk of fracture with a recent addition to its licence to include all patients with hip fracture. It is given as a slow intravenous infusion, with patients needing analgesia to help postdose influenza-like symptoms that last for around three days. The significantly increased risk of serious atrial fibrillation reported in one of the HORIZON studies requires further study and should be monitored in clinical practice.
References
1. Perry C M, Figgett DP. Drugs 2004;64:1197-1211.
2. Reid IR, Miller P, Lyles K, et al. N Engl J Med 2005;353:898-908.
3. Woolf AD, St John Dixon A. Osteoporosis: a clinical guide. 2nd ed. London: Martin Dunitz; 1998.
4. Compston JE, Rosen CJ. Fast facts: osteoporosis. 5th ed. Oxford: Health Press; 2006.
5. van Staa TP, Kanis JA, Geusens P, et al. Value Health 2007;10(5):348-57.
6. Allen MR. Expert Opin Drug Metab Toxicol 2008;11:1371-8.
7. Laroche M. Am J Med 2008;121(9):744-7.
8. Black DM, Delmas PD, Eastell R, et al. N Engl J Med 2007;356(18):1809-21.
9. Lyles KW, Colon-Emeric CS, Magaziner JS, et al. N Engl J Med
2007;357(18):1799-1809.
10. Ishida Y, Mine T, Taguchi T. Effect of progestins with different glucocorticoid activity on bone metabolism. Clin Endocrinol (Oxf) 2008; 68(3):423-8.
11. Lopez LM, Grimes DA, Schulz KF, Curtis KM. Steroidal contraceptives: effect on bone fractures in women. Cochrane
Database Syst Rev 2009;15(2):CD006033.
12. Kaunitz AM, Arias R, McClung M. Bone density recovery after medroxyprogesterone acetate injectable contraceptive use.
Contraception 2008;77(2):67-76.
13. National Institute for Health and Clinical Excellence. Health
Technology Appraisal No.160. Osteoporosis — primary prevention. http://www.nice.org.uk/Guidance/TA160. Accessed 9 Jan 2009.
14. National Institute for Health and Clinical Excellence. Health Technology Appraisal No.161. Updated: Osteoporosis — secondary prevention.
http://www.nice.org.uk/Guidance/TA161. Accessed 9 Jan 2009.
15. Compston J. N Engl J Med 2007;356(18):1878-80.
16. McClung M, Recker R, Miller P, et al. Bone 2007;41:122-8 .
17. Assessment of fracture risk and its application to screening
for postmenopausal osteoporosis. Report of a WHO Study Group. WHO technical report series 1994;843:1-129.
18. Saag K, Lindsay R, Kreigman A, et al. Bone 2007;40:1238-43.