teaser
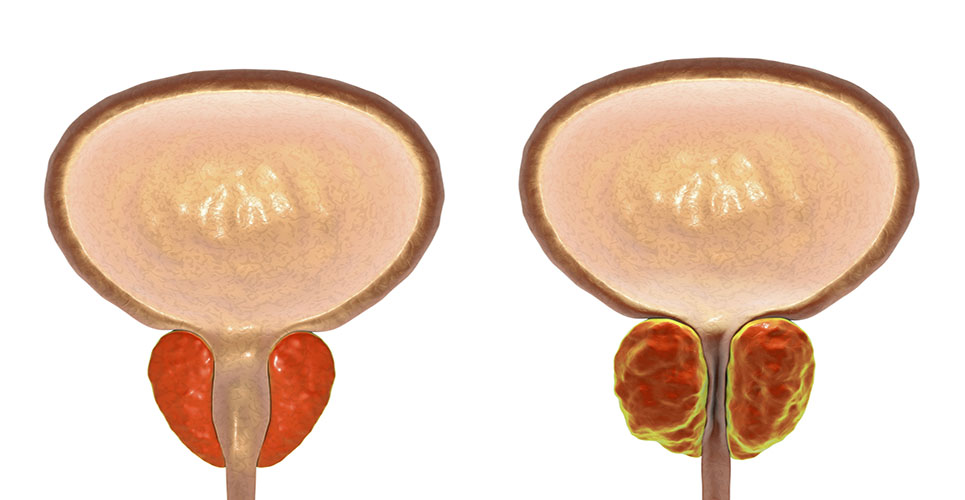
Therapies under development to treat prostate cancer by inhibiting the ability of insulin-like growth factor (IGF-1) to activate its target receptor could have unexpected results, especially if a major tumour suppressor gene – p53 – is already compromised, according to new research by investigators at Fred Hutchinson Cancer Research Center.
IGF-1 is a polypeptide hormone that can influence growth, differentiation and survival of cells expressing the type 1 receptor (IGF-1R).
Past clinical, epidemiological and experimental studies have strongly implicated IGF-1 as a contributing factor in the natural history of prostate cancer. However, very little has been done to prove absolutely that the expression or activation of the IGF-1 signalling pathway at physiologically relevant levels is sufficient to cause a healthy prostate cell to become a cancer cell.
Norman Greenberg, PhD, and colleagues conducted a pair of experiments by manipulating gene expression directly in the epithelial compartment of the mouse prostate gland to better understand the role of IGF-1R.
In contrast to studies that correlated elevated levels of IGF-1 with the risk of developing prostate cancer, Greenberg’s research showed that eliminating IGF-1R expression in an otherwise normal mouse prostate caused the cells to proliferate and become hyperplastic.
Published in the 1 May edition of Cancer Research, the study supports a critical role for IGF-1R signalling in prostate tumour development and identifies an important IGF-1R-dependent growth control mechanism, according to the authors.
“If our predictions hold true, tumour cells with intact p53 may show the best response to therapy targeting the IGF-1R signal, however when p53 is not functioning normally, response to this therapy may not be as expected,” said Greenberg, the study’s corresponding author and a member of the Hutchinson Center’s Clinical Research Division.
Greenberg’s message to clinicians who administer IGF-R1 therapy: “We’re all hoping for good results but let’s proceed with caution.”
Fred Hutchinson Cancer Research Center