A wealth of evidence indicates that ePrescribing and Medicines Administration systems deliver benefits but they need good implementation and ongoing support to gain full benefit.
The use of medicines is the most common therapeutic intervention used in medicine and plays a vital role in managing chronic conditions and curing disease. Medicines represent the biggest budget item of NHS expenditure after staff costs. Reports to the National Reporting and Learning System (NRLS) indicate that medicines related issues are the second most common report of harm, after falls. Within this context it is unsurprising that medicines optimisation is a key issue for the NHS.
The optimisation of the use of medicines requires that the ‘best’ medicine is used to manage a patient’s disease in the most appropriate manner. This starts with the correct diagnosis and flows on to appropriate medication selection; appropriate in this sense meaning a medicine that best suits the patient and meets his or her medication needs.
Information technology can assist in the delivery of medicines optimisation in a number of ways; by reducing medication related risk; by promoting adherence with policy; and by allowing organisations to change the way care is delivered; releasing clinical staff to more patient focussed roles as suggested by the Carter Review.1
Optimising medicines from diagnosis to consumption
Although the focus of medicines optimisation is understandably on medicines; the very beginning of the process lies in supporting the clinician in arriving at a suitable diagnosis. A UK-produced diagnosis support tool, Isabel, has been used in a number of hospitals to support differential diagnosis and may represent a future integrated decision support process for the UK.
Whilst pharmacy has used technology to manage stock control for many years, this can still be improved. The optimum process is completely digital and makes full use of automation, where appropriate. The introduction of the Falsified Medicines Directive offers a number of opportunities to further streamline the supply of medicines with the potential for full traceability of specific packs to individual patients. The majority of focus is however on electronic prescribing and medicines administration systems; the reduction of medication related error and the opportunities for change in the processes to support medicines optimisation.
Incidence of medication related problems
One of the earliest papers to examine medication related incidents identified 6.5 actual and 5.5 potential adverse drug events per 100 admissions, a significant number of which were preventable. The majority of the preventable adverse events were associated with medication ordering (56%) or administration (34%).2
It is important to note that whilst many prescribing errors are captured by subsequent pharmacist or nurse review, there are few opportunities to ‘capture’ errors at the administration stage. In this context, it is unsurprising that a review of voluntary reports to the national reporting and learning service identified that the majority (over 56%) of the reports of medication incidents resulting in severe harm or death were related to medicines administration.3
Prescribing error remains a significant issue however, as evidenced in a UK study of medication errors, which identified 1025 prescribing errors in 974 of 6605 medication orders (14.7%). Contributing factors included lack of feedback on errors, poor documentation and communication of prescribing decisions, and lack of information about patients’ medication histories from primary care.4
A recent investigation of the incidence of ‘in-hospital’ adverse drug reactions (as opposed to errors) in 3695 patient episodes identified that 545 (14.7%) were associated with one or more ADRs, half of which were identified as avoidable. These ADRs resulted in a greater length of stay (20 days versus 8 days) and higher mortality rates than for patients without ADRs (10.7% versus 3.9%) and may represent an ‘additional’ risk to any harm due to medication error. Some, or all of these ADRs may be mitigated by IT.
Reduction in prescribing errors
A number of studies from around the world have shown that electronic prescriptions are associated with fewer errors than handwritten prescriptions. Legibility and completeness of the necessary data items is invariably improved markedly by the use of ePrescribing systems.6–8 Indeed one of the most common user complaints is that electronic systems require greater level of data input than they were used to with ‘paper’ systems, which may in itself contribute to risk (see ‘cognitive load’ later).
But ePrescribing systems provide more than just improvements in legibility. Experience in one US hospital, over a four-year period, was of a fall in medication errors of 81% following the introduction of an ePrescribing and Medicines Administration (ePMA) system with integrated decision support. Reductions were seen in errors related to dose, frequency and route selection as well as in errors involving allergies.9
A more recent before and after study of two different commercial systems implemented in two Australian teaching hospitals and involving medication chart audit of 3291 admissions showed significant reductions in medication error;10 with a decline in errors at Hospital A from 6.25 per admission to 2.12 and at Hospital B from 3.62 to 1.46.
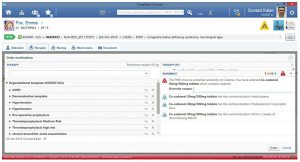
For demonstration purposes only
Reducing medicines administration error
In a study of 14,041 administration events a 41.4% relative reduction in errors (from 11.5% to 6.8%) with a 50% relative reduction in the rate of potential adverse drug events was observed when administration was supported by the use of barcodes. There was a 27% reduction in the rate of timing errors and transcription errors were completely eliminated.11
One UK study of a ‘closed loop’ ePMA system, where barcode verification was used to confirm both patient identity and medication selection, found a reduction in prescribing error from 3.8% to 2%; a 24% reduction in administration error and an improvement of over 60% in the checking of patient identity prior to administration of medicines.12 An interesting observation was that during the pre-intervention baseline measurement, 22% of medication charts were unavailable for review, an issue that is eliminated by electronic systems.
Improving medication choice
‘Guided’ prescribing, the use of pre-defined orders to support the selection of medicines in line with local policy or national guidelines, has been shown to improve formulary compliance and improve the selection of appropriate dose and frequency choices.4,13 The use of an ‘antibiotic manager’ system, at LDS Hospital in Salt Lake, improved antimicrobial choices,14 with reductions in excessive dosages, antibiotic susceptibility mismatches, reduction in excessive duration of treatment and reductions in cost. A reduction in orders to which the patient had a documented allergy and a significant reduction in adverse events caused by anti-infective agents were also reported.
System mediated medication error
Whilst ePMA systems can reduce the incidence of medication related error, the picture is not universally positive and the implementation of ePMA systems can cause errors, which tend to be ‘different’ from non-system errors.
- Deployment
Some errors are unrelated to the system itself but are caused by the way the system is implemented. For example, in one implementation in a paediatric intensive care unit, medicines were unavailable from the automated cabinets until a prescription had been written and doctors could not write prescriptions until the patient had been admitted ‘onto the system’; so doctors had to spend time waiting to write prescription orders rather than caring for these critically ill infants. This led to an increase, rather than the expected decrease in mortality.15
- Usability
Common sources of error are associated with ‘cognitive load’ where the prescriber or nurse needs to ‘remember’ to do something in the ePMA system that was not needed in the ‘paper’ system.16 This is a particular issue with the delay between the ‘current’ time of day and the scheduled time of the first dose; where morning doses written after the normal morning administration time will not be scheduled until the next day, unless the prescriber adds a ‘STAT’ dose. The use of ‘multiple’ processes; such as separate paper ‘charts’ or indeed multiple ePrescribing systems for complex prescriptions, including step up or step down doses, warfarin or infusions; also leads to error with a particular risk of omitted doses.17
Mistakes in selection from drop down menus also presents significant opportunity for error and availability of long lists of medicines or complete ‘order sentences’, although often preferred by users, (who want the minimum number of ‘clicks’ possible), increase the incidence of selection error.18 The National Patient Safety Agency (NPSA) in collaboration with the Common User Interface (CUI) programme identified methods to reduce some of these system-related errors.19
ePMA and streamlined pharmacy services
The use of ePMA systems not only improves legibility and completeness of prescriptions but also improves availability of information. A number of studies have noted that the availability of medication charts is an issue with paper processes and the ‘available to everyone at all times’ nature of electronic systems facilitates the transformation of services with associated cost reductions.
One study examined the impact of an ePMA system on the work of clinical pharmacy staff, noting that in the hospital with ePMA, pharmacists spent 70% of their ward time on clinical activities compared with less than 30% in other hospitals.20 The cost of transmitting the need to supply a medicine from the ward to the pharmacy was also investigated and found to be 16p per order with ePMA compared with 43.8p per order with manual systems.21
Integration of ePMA with stock control and automated dispensing has been showcased at Sunderland Royal Hospital, with the elimination of dispensing errors (for automatically dispensed items),22 reductions in inventory costs, and reduced dispensing turnaround times. A review of dispensary skill-mix and redeployment of some resources to other duties has also been facilitated, which is just what is anticipated by the Carter review.1
Key points
- Information technology can support medicines optimisation from the outset by facilitating appropriate diagnosis and supporting the appropriate medication choice.
- Prescribing and administration errors are minimised improving the safety of medication use for patients and reducing transaction costs but care is needed in system design and implementation to prevent the introduction of unforeseen risks and usability problems.
- Reviewing and transforming care processes allows better use of skill mix and improved focus on patient care.
Authors
Keith Farrar BSc MPharm
Ann Slee BPharm MSc MRPharmS
Digital Technology Patients and Information Directorate, NHS England
Email: [email protected]
References
- Lord Carter of Coles. Operational productivity and performance in English NHS acute hospitals: Unwarranted variations. An independent report for the Department of Health. February 2016.
- Bates DW et al. Incidence of Adverse Drug Events and Potential Adverse Drug Events Implications for Prevention. JAMA 1995;274:29–34.
- Cousins D, Gerrett D, Warner B. A review of medication incidents reported to the National Reporting and Learning System in England and Wales over six years (2005 – 2010). Br J Clin Pharmacol. 2011 Dec 22. doi: 10.1111/j.1365-2125.2011.04166.x. [Epub ahead of print].
- Franklin BD et al. Prescribing errors in hospital inpatients: a three-centre study of their prevalence, types and causes. Postgrad Med J 2011;87(1033):739–45.
- Davies EC et al. Adverse Drug Reactions in Hospital In-Patients: A Prospective Analysis of 3695 Patient-Episodes. PLoS ONE 2009;4(2):e4439.
- Hughes DK, Farrar KT, Slee AL. The trials and tribulations of electronic prescribing. Hosp Presc Eur 2001;1:74–6.
- Ammenwerth E et al. The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. J Am Med Inform Assoc 2008;15(5):585–600.
- Jimenez Munoz AB et al. Comparison of medication error rates and clinical effects in three medication prescription-dispensation systems. Int J Health Care Qual Assur 2011;24(3):238–48.
- Bates DW et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc 1999;6(4):313–21.
- Westbrook JI et al. Effects of Two Commercial Electronic Prescribing Systems on Prescribing Error Rates in Hospital In-Patients: A Before and After Study. PLoS Med 2012;9(1):e1001164.
- Poon EG, Keohane CA, Yoon CS, Ditmore M, Bane A et al. Effect of Bar-Code Technology on the Safety of Medication Administration. N Engl J Med 2010;362:1698–707.
- Franklin BD et al. The impact of a closed-loop electronic prescribing and administration system on prescribing errors, administration errors and staff time: a before-and-after study Qual Saf Health Care 2007;16:279–84.
- Farrar K et al. Use of structured paediatric-prescribing screens to reduce the risk of medication errors in children. Br J Healthcare Comput Info Manage 2003; 20(4): 25-7
- Evans RS et al. A computer-assisted management program for antibiotics and other anti-infective agents. N Engl J Med 1998;338(4):232–8.
- Han YY et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 2005;116(6):1506–12.
- Koppel R et al. Facilitating Medication Errors Role of Computerized Physician Order Entry Systems in Facilitating Medication Errors. JAMA 2005;293:1197–1203
- Palchuk M et al. An unintended consequence of electronic presciptions: prevalence and impact of internal discrepancies. J Am Med Inform Assoc 2010;17:472–6.
- Westbrook JI et al. The safety of electronic prescribing: manifestations, mechanisms, and rates of system-related errors associated with two commercial systems in hospitals. J Am Med Inform Assoc. doi:10.1136/amiajnl-2013001745.
- National Reporting and Learning Service. Design for patient safety: guidelines for the safe on-screen display of medication information | 2010-02 | v1.
- Abu Zayed L, Farrar K, Mottram D. Time spent on drug supply activities in UK hospitals Am J Health-Syst Pharm 2000;57:2006-7
- Abu-Zayed LA, Farrar K, Mottram DR. Comparative evaluation of systems for drug supply to hospital wards in the United Kingdom. J Soc Adm Pharm 2001;18:136–42.
- Beard R. e-Prescribing and robotic dispensing: part I. Hosp Pharm Eur 2014;72.

