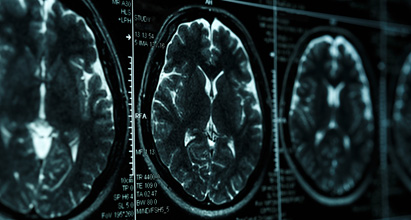
Researchers have devised a new drug delivering nanoparticle that could provide a better way to treat glioblastoma.
The particles, which carry two different drugs, are designed so that they can easily cross the blood-brain barrier and bind directly to tumour cells. One drug damages tumour cells’ DNA, while the other interferes with the systems cells normally use to repair such damage.
In a study of mice, the researchers showed that the particles could shrink tumours and prevent them from growing back.
Researchers have devised a new drug delivering nanoparticle that could provide a better way to treat glioblastoma.
The particles, which carry two different drugs, are designed so that they can easily cross the blood-brain barrier and bind directly to tumour cells. One drug damages tumour cells’ DNA, while the other interferes with the systems cells normally use to repair such damage.
In a study of mice, the researchers showed that the particles could shrink tumours and prevent them from growing back.
Paula Hammond, a David H. Koch professor in engineering, the head of (MIT) department of chemical engineering and a member of MIT’s Koch Institute for Integrative Cancer Research, said: “What is unique here is we are not only able to use this mechanism to get across the blood-brain barrier and target tumors very effectively, we are using it to deliver this unique drug combination.”
Ms Hammond and Scott Floyd, a former Koch Institute clinical investigator who is now an associate professor of radiation oncology at Duke University School of Medicine, are the senior authors of the paper, which appears in Nature Communications. The paper’s lead author is Fred Lam, a Koch Institute research scientist.
The nanoparticles used in this study are based on particles originally designed by Ms Hammond and former MIT graduate student Stephen Morton, who is also an author of the new paper. These spherical droplets, known as liposomes, can carry one drug in their core and the other in their fatty outer shell.
To adapt the particles to treat brain tumors, the researchers had to come up with a way to get them across the blood-brain barrier, which separates the brain from circulating blood and prevents large molecules from entering the brain.
The researchers found that if they coated the liposomes with a protein called transferrin, the particles could pass through the blood-brain barrier with little difficulty. Transferrin also binds to proteins found on the surface of tumor cells, allowing the particles to accumulate directly at the tumor site while avoiding healthy brain cells.
This targeted approach allows for delivery of large doses of chemotherapy drugs that can have unwanted side effects if injected throughout the body. Temozolomide, which is usually the first chemotherapy drug given to glioblastoma patients, can cause bruising, nausea, and weakness, among other side effects.
Researchers built on prior work from Mr Floyd and Michael Yaffe, a David H. Koch professor of science and member of the Koch Institute – who is also an author of the paper – on the DNA-damage response of tumours. They packaged temozolomide into the inner core of the liposomes, and in the outer shell they embedded an experimental drug called a bromodomain inhibitor. Bromodomain inhibitors are believed to interfere with cells’ ability to repair DNA damage.
By combining these two drugs, the researchers created a ‘one-two punch’ that first disrupts tumor cells’ DNA repair mechanisms, then launches an attack on the cells’ DNA while their defenses are down.
The researchers tested the nanoparticles in mice with glioblastoma tumors and showed that after the nanoparticles reach the tumor site, the particles’ outer layer degrades, releasing the bromodomain inhibitor JQ-1. About 24 hours later, temozolomide is released from the particle core.
Their experiments revealed that drug-delivering nanoparticles coated with transferrin were far more effective at shrinking tumors than either uncoated nanoparticles or temozolomide and JQ-1 injected into the bloodstream on their own. The mice treated with the transferrin-coated nanoparticles survived for twice as long as mice that received other treatments.
In the mouse studies, the researchers found that animals treated with the targeted nanoparticles experienced much less damage to blood cells and other tissues normally harmed by temozolomide.
The particles are also coated with a polymer called polyethylene glycol (PEG), which helps protect the particles from being detected and broken down by the immune system. PEG and all of the other components of the liposomes are already FDA-approved for use in humans.
Researchers said JQ-1, the bromodomain inhibitor used in this study, would likely not be well-suited for human use because its half-life is too short, but other bromodomain inhibitors are now in clinical trials.
They anticipate this type of nanoparticle delivery could also be used with other cancer drugs, including many that have never been tried against glioblastoma because they couldn’t get across the blood-brain barrier.
“Because there’s such a short list of drugs that we can use in brain tumors, a vehicle that would allow us to use some of the more common chemotherapy regimens in brain tumors would be a real game-changer,” Mr Floyd says.
“Maybe we could find efficacy for more standard chemotherapies if we can just get them to the right place by working around the blood-brain barrier with a tool like this.”
The research was funded by the Koch Institute Frontier Research Program; a KI Quinquennial Cancer Research Fellowship; the Bridge Project, a partnership between the Koch Institute and the Dana-Farber/Harvard Cancer Center; and the Koch Institute Support (core) Grant from the National Cancer Institute.