Stuart Semple
MSc MRPharmS
Principal Pharmacist Clinical Services
University Hospital Lewisham
London, UK
E:[email protected]
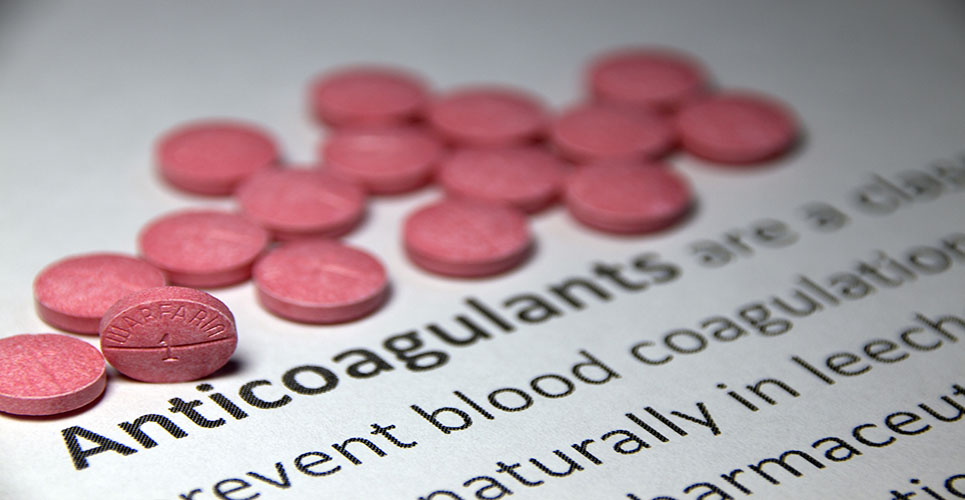
Non-rheumatic atrial fibrillation is now the most common indication for patients seen in anticoagulant clinics, comprising 30–50% of total patient numbers. Advances in technology to allow immediate reporting of International Normalised Ratio (INR) using a fingerprick method of sampling capillary blood have resulted in an increased capacity of clinics to monitor patients taking anticoagulants.
Pharmacist-led anticoagulation clinics
Traditionally, outpatient anticoagulation clinics have been staffed by a junior member of the medical team, but in the last 10 years this task has been delegated to clinical pharmacists, as part of a more general drive towards pharmacy involvement in ambulatory care. A typical structure for pharmacist-led anticoagulation is for the consultant in charge of haemophilia or haematology to retain overall responsibility for anticoagulation management. The clinical pharmacist consults with individual patients after a laboratory technician measures their INR. Administrative staff are responsible for the management of appointments and some clinics also benefit from nursing support.
The role of the clinical pharmacist in the anticoagulation clinic includes:
- Adjusting doses of anticoagulants in response to INR and changes in the patient’s drug regimen or state of health.
- Promoting concordance with treatment and a healthy lifestyle while taking therapy.
- Prescribing low-molecular-weight heparin (LMWH) for high-risk patients who are seriously underanticoagulated. This could include patients with newly diagnosed thrombosis or who are at high risk of thromboembolic disease, such as those with mechanical heart valves.
- Liaising with other healthcare professionals.
- Referring difficult cases to a member of the medical team (see Table 1).
[[HPE01_table1_36]]
Audits of pharmacist-led anticoagulation clinics have shown this model of care is equally effective in maintaining anticoagulation within the therapeutic range.(1) Additional benefits of pharmacy input to this group of patients are:
- Knowledge of pharmacokinetics and drug interactions with anticoagulants.
- A wider appreciation of non-prescribed treatments, such as over-the-counter and herbal remedies.
- Junior doctors who are delegated to manage anticoagulation clinics generally rotate more frequently than pharmacists do. Consistency of personnel allows rapport to be developed with patients. Also, anecdotal reports suggest that anticoagulation is viewed by junior doctors as unexciting and repetitive.
- The clinical pharmacy team can provide an effective link between inpatient and outpatient care.
Protocols and documentation
Extending the roles of non-medical staff in any aspect of clinical care requires robust procedures to ensure optimum and safe practice. The roles of each member of the team have generally been defined in a Standard Operational Procedure (SOP). This document would also define the INR for each treatment indication, standards for dosage adjustment, time intervals between appointments and clear criteria for referral to medical staff.
The situation has changed recently following publication in the UK of the Crown Report,(2) a document recommending clear guidelines for extending the practice of any member of staff in the prescribing, administration or supply of medicines for a defined group of patients, in this case those taking anticoagulants. This has now been underpinned with a legislative framework. In short, SOPs should be rewritten as Patient Group Directions (PGDs), where non-medical staff operate as prescribers following a diagnosis from a doctor (dependent prescriber).
Future developments
Nurse management
The current shortage of pharmacists has forced pharmacy managers to prioritise the deployment of their service. There is a proportion of patients taking anticoagulants who are very stable on therapy and require very little input at each visit. Under a PGD, it would be possible for nursing staff to carry out similar roles to clinical pharmacists, particularly where the patient was stable and the skills of the pharmacist were not required. Pharmacy technicians could also carry out this task.
Outpatient management of deep vein thrombosis
Management of patients suffering from deep vein thrombosis (DVT) is increasingly being carried out on an outpatient basis, mainly because of the flexibility offered by the once-daily subcutaneous dosing schedule of LMWH. Management of these patients in the early days following diagnosis can be coordinated through the pharmacy department, and pharmacists can be trained to administer LMWH injections.
Primary care anticoagulation clinics
Part of the strategy for the NHS in the UK is for care to be more focused on the community and more specifically on the patient’s general practitioner (GP). Some hospital-based anticoagulant services are carrying out routine monitoring in GP practices. This is feasible because of the portable nature of the testing equipment. A PGD would have to be written to support this which would include clear guidance on which body was responsible for clinical management of patients. For clinical pharmacists working in the hospital setting, this opens up the possibility for wider medicines management advice for doctors and their patients in the community.
Home monitoring of International Normalised Ratio
Further advances in technology have led to INR testing devices which can be used by patients at home. These work in a similar way to blood sugar monitoring systems. The patients must be carefully chosen, and this would be defined in the PGD. The role of the anticoagulant clinic in this situation would be to offer a calibrating service for the measuring devices and education services for patients to manage their own dosing of anticoagulants, with much less frequent review visits to the clinic itself.
Conclusion
Outpatient management of anticoagulation is increasingly being delegated to non-medical staff. Professions other than pharmacy may be able to participate in this activity. Clear policies must be in place to ensure safe and effective therapy for patients and to ensure that a medicolegal framework supports staff in carrying out these extended roles.
References
- Ellis RF, Stephens MA, Sharp GB. Evaluation of a pharmacy-managed warfarin-monitoring service to coordinate inpatient and outpatient therapy. Am J Hosp Pharmacy 1992;49:387-94.
- Department of Health, Crown J. Report of the Advisory Group on Nurse Prescribing [Crown Report]. London: Department of Health; 1989.
Resource
NHS Executive Guide to Approved Group Protocols
W:www.groupprotocols.org.uk
Further reading
Fleming HA, Bailey SM. Mitral valve disease, systemic embolism and anticoagulants. Postgrad Med J 1971;47:599 -604
Stroke Prevention in Atrial Fibrillation Investigators.
Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke Prevention in Atrial Fibrillation III randomised clinical trial. Lancet 1996;348:633-8