GHJ Mickisch
MD PhD FRCS(NL)
Professor
Department of Urology
Erasmus Medical Center Rotterdam The Netherlands
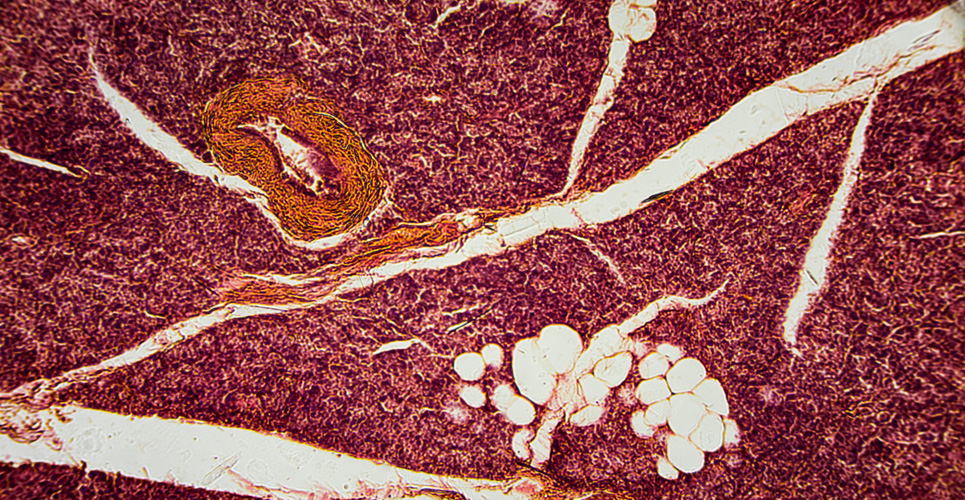
Although surgery is the mainstay of tumour therapy in localised renal cell carcinoma (RCC), tumour nephrectomy in a metastatic situation remains highly controversial. To address the issue of whether a cytoreductive tumour nephrectomy before interferon beta-based immunotherapy is superior to interferon beta alone in terms of time to progression and overall survival, the EORTC-GU group embarked on a randomised phase III study (EORTC 30947).
[[HPE03_fig1_14]]
Methods
Eighty-five patients were included from June 1995 to July 1998. Two proved to be ineligible, one on each treatment. Of the remaining 83, 41 were randomised to combined treatment (arm 1) and 42 to receive immunotherapy alone (arm 2). All patients had a histologically proven metastatic RCC, were progressive at entry, and signed informed consent. In the case of therapy 1, surgery was performed within four weeks after randomisation, and immunotherapy started between two and four weeks after the day of the operation. In the case of therapy 2, immunotherapy started within one working day after randomisation. Follow-up visits were monthly with a projected treatment duration of one year. Dosage of interferon beta was 5 ¥ 106 units/m(2), three times a week. An intent-to-treat analysis was done.
Findings
Patients were evenly divided between arms 1 and 2 with respect to age, sex, WHO performance score (0.1), tumour type, grade, venous invasion, lung mets only (stratification factor), liver mets, bone mets and co-morbidity. Twenty patients were younger than 50 years and 12 patients older than 70 years. Four patients in arm 1 received no tumour nephrectomy and went on immunotherapy only whenever possible. There were six perioperative surgical complications, and only one of these patients did not receive immunotherapy. Toxicity, such as myelotoxicity, nausea, anorexia, and neurological/psychological disorders, was equally distributed between treatment arms and led to a dose modification in 32% of evaluable patients. Fifty per cent of patients received more than 16 weeks of interferon beta treatment. There were five CRs (complete responses) in arm 1. The one and only CR in arm 2 was then taken off protocol and received a tumour nephrectomy. He is still in CR at two years of follow-up.
Partial responses and stable diseases were similarly distributed between treatment arms. Both endpoints, time to progression (logrank p=0.04) and duration of survival (logrank p=0.03), were in favour of treatment arm 1. The median survival shifted from seven months (arm 2) to 17 months (arm 1).
Interpretation
In the context of interferon beta-based immunotherapy, prior cytoreductive tumour nephrectomy significantly delays time to progression and improves on overall survival in metastatic RCC patients presenting with a good performance status.