Adding an arginine-depleting agent to chemotherapy extends survival for patients with advanced non-epithelial pleural mesothelioma, a randomised controlled trial suggests.
The ATOMIC-Meso trial is the continuation of 20 years of research at Barts Cancer Institute at Queen Mary University of London, that began with the discovery that malignant mesothelioma cells lack the argininosuccinate synthetase 1 (ASS1) protein, which enables cells to manufacture their own arginine.
Pegargiminase (ADI-PEG20), a first-in-class arginine-depleting agent, degrades arginine into citrulline and ammonia, starving tumour cells that lack ASS1 of the essential amino acid.
For the global phase three trial, 249 patients with advanced non-epithelial pleural mesothelioma were randomised to treatment with pegargiminase and standard platinum and pemetrexed chemotherapy or a matched placebo plus chemotherapy.
During the study, which was sponsored by Polaris Pharmaceuticals and published in the journal JAMA Oncology, patients with advanced non-epithelial pleural mesothelioma either received weekly intramuscular pegargiminase (36.8 mg/ m2) or placebo.
All patients received intravenous pemetrexed (500 mg/m2) and platinum (75-mg/m2 cisplatin or carboplatin area under the curve 5) chemotherapy every three weeks for up to six cycles.
Pegargiminase or placebo was continued until progression, toxicity, or 24 months.
Randomised patients had a mean age of 65.6 years, and the majority (82.7%) were male.
Overall survival was significantly longer in the pegargiminase group (median 9.3 months) than in the placebo group (median 7.7 months), the study authors reported, equating to a 29% lower risk of death in the pegargiminase group.
‘A therapeutic plateau was reached by 36 months with three- to four-fold more patients alive in the pegargiminase group compared with the placebo group (11.9% vs 3.3%),’ they added.
The pegargiminase group also had a 35% lower risk of mesothelioma progression compared with the placebo group.
Of note, around 5% of the pegargiminase group but none of the placebo group completed two years of weekly therapy, highlighting a subgroup with ‘exquisite sensitivity’ to arginine depletion that warranted further investigation, the researchers suggested.
Pegargiminase-based chemotherapy was well tolerated, with no new safety signals, they added.
‘Recently, the mesothelioma therapeutic landscape has shifted to favour immune checkpoint blockade over platinum-based chemotherapy,’ the researchers wrote.
‘While not replacing frontline immunotherapy with the more modest survival improvement in the ATOMIC-Meso study, pegargiminase nonetheless provides an incremental chemotherapeutic advance for patients with essentially chemotherapy-refractory non-epithelioid disease.’
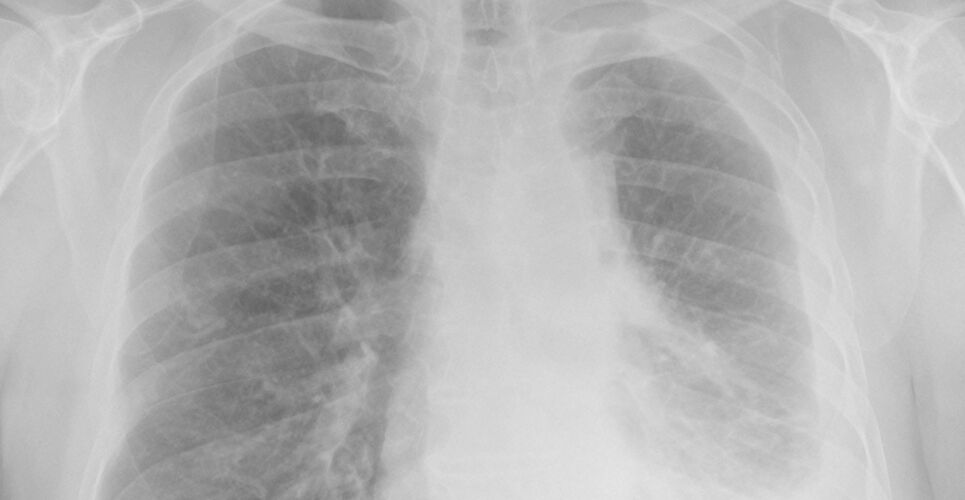
Malignant pleural mesothelioma has among the lowest five-year survival rate of any solid cancer, estimated at 5% to 10%, the researchers noted.
The novel data added further impetus to the field of cancer metabolism, the researchers said, particularly strategies targeting specific amino acids.
Lead author Professor Peter Szlosarek, professor of medical oncology and group leader at the Barts Cancer Institute at Queen Mary University of London, first discovered that malignant mesothelioma cells lack ASS1.
Professor Szlosarek said: ‘This discovery is something I have been driving from its earliest stages in the lab, with a new treatment now improving patient lives affected by mesothelioma.
‘It’s truly wonderful to see the research into the arginine starvation of cancer cells come to fruition.’
Ongoing studies are assessing pegargiminase in patients who have sarcoma or glioblastoma multiforme and other cancers dependent on arginine.
Previous research has suggested that use of the immunotherapy nivolumab significantly improves overall survival in malignant mesothelioma with evidence of disease progression.