AbbVie’s bispecific antibody treatment epcoritamab (brand name Tepkinly) has been recommended by the National Institute for Health and Care Excellence (NICE) to treat relapsed or refractory (R/R) diffuse large B-cell lymphoma (DLBCL) – the first bispecific to be given as a subcutaneous injection.
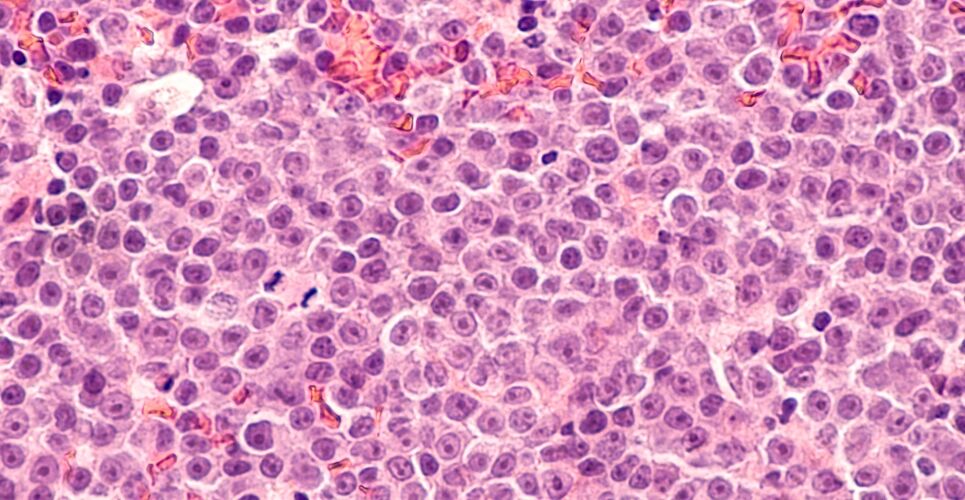
DLBCL is an aggressive blood cancer with nearly 5,500 new diagnoses in the UK each year, and poor prognosis for some 700 of these patients who have R/R DLBCL.
The new recommendation means adults with DLBCL whose cancer has returned or has not responded to at least two previous treatments, and who have previously had polatuzumab vedotin or it is contraindicated or not tolerated, will have access to epcoritamab subcutaneous bispecific treatment option administered in a hospital setting.
This follows the granting of conditional marketing authorisation by the UK’s Medicines and Healthcare products Regulatory Agency in October 2023 and by the European Commission in late September 2023.
Epcoritamab and capacity planning
In contrast to some existing therapeutic options, which are administered intravenously, epcoritamab does not require cell collection and engineering.
The treatment is given by a blood cancer specialist doctor or nurse to eligible patients weekly for 12 weeks, then every other week for 24 weeks (12 injections), before continuing as one injection every four weeks until treatment is discontinued, either due to cancer progression or side effects.
Eligible patients can start epcoritamab therapy after appropriate premedication has been administered and monitoring for adverse events is available. Patients stay in hospital for 24 hours after the first full dose to monitor for side effects.
Professor Chris Fox, professor of haematology at the University of Nottingham’s School of Medicine and honorary consultant haematologist at Nottingham University Hospitals NHS Trust, said: ‘Despite recent therapeutic advances, treatment options for this hard-to-treat group of patients have been limited.
‘This can mean many patients do not have suitably effective treatment options, resulting in a poor prognosis. [This] decision by NICE on epcoritamab gives patients and clinicians an additional choice of administration option, which may help to support capacity planning within lymphoma services.’
He added: ’The decision by NICE will be welcomed by both patients and the clinical community.’
EPCORE NHL-1 trial
The NICE recommendation is based on data from the single-arm, open-label, multicentre safety and preliminary efficacy phase 1/2 EPCORE NHL-1 trial,
The trial demonstrated a 62% (n=86/139) overall response rate, meaning 62% of participants’ blood cancer either went down by half (partial response) or showed no evidence of disease from tests and scans (a complete response).
The complete response rate was 39% (n=54/139), meaning there was no evidence of disease from tests and scans in 39% of these hard-to-treat patients, who on average had already been through three types of treatment before starting the trial.
In the Phase 1/2 NHL-1 clinical trial, epcoritamab prevented growth or spread of the cancer for an average of 15.6 months, and the patients lived for an average of 19.4 months from the start of epcoritamab therapy.
The most common adverse reactions of any grade (≥20%) observed in the trial were cytokine release syndrome (50.9%), fatigue (30.5%), neutropenia (30.5%), injection-site reactions (29.9%), abdominal pain (23.4%), pyrexia (23.4%), nausea (21.6%) and diarrhoea (21.0%).
Commenting on the NICE recommendation, Rincy George, policy officer at Blood Cancer UK, said: ‘Like many that experience blood cancer, people with relapsed or refractory DLBCL experience anxiety around the prospect of not responding to treatment or the cancer once again returning.
’Today’s decision from NICE approving epcoritamab for eligible patients for use on the NHS in England and Wales is a welcome step for many.’