A study has revealed how cancer cells either shrink or super size during drug therapy or other environmental challenges to enable survival
In a study published in Science Advances, researchers from the institute of Cancer research in London, showed that melanoma cancer cells will either shrink or become super sized as a survival mechanism in the face of either drug treatment or any other challenges that might occur within their environment.
Although it is acknowledged that there are differences in the size of cell types, there is also a recognition that for proliferating cell types, there is little variation in cell size. This implies that there is some mechanism or checkpoint, responsible for ensuring that cells maintain a particular size during the proliferative phase. Clearly, this checkpoint is disturbed in cancer and it is known that cancers will arise due to the accumulation of mutations in genes and which alter the normal proliferation, differentiation and death process.
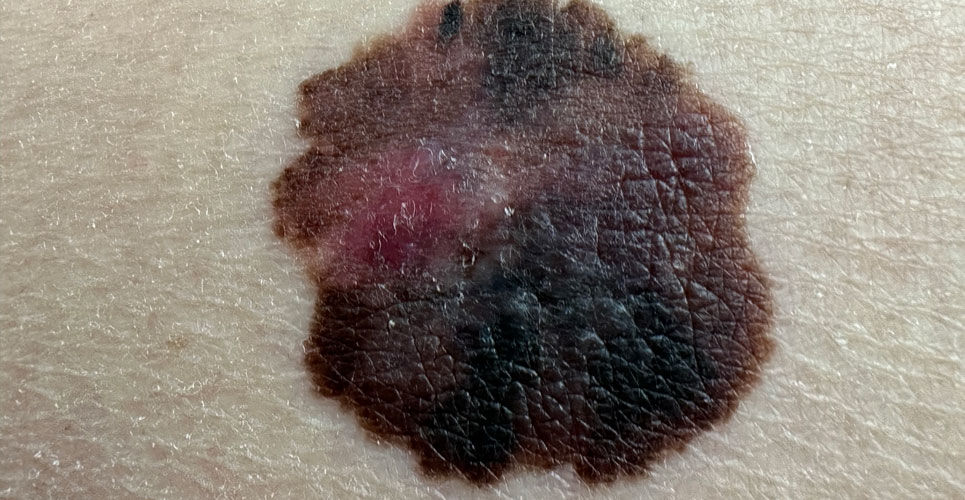
In the current Science Advances study, researchers used a combination of biochemical profiling and mathematical analyses, to examine how genetic changes affect the size of cancer cells. They focused on skin melanoma cells which are known to be driven by two genetic mutations, a BRAF gene (60%) and an NRAS mutation (20 – 30%) and examined differences in the size and shape of these cells with the two mutations.
Interestingly, the team found that BRAF-mutant cancer cells were very small, whereas NRAS-mutant cells were much bigger and larger still, when the cells were drug resistant. It seemed that small cells were able to better tolerate DNA damage, due to high concentrations of DNA repair proteins such as PARP, BRCA1 or ATM1.
The researchers believed that their findings might help clinicians to decide upon the choice of treatment. For instance, small cells were likely be more vulnerable to PARP inhibitors, i.e., drugs affecting the proteins responsible for DNA repair. In contrast, the larger NRAS-mutant cells, already had lots of DNA damage, which the cells were unable to repair and hence unlikely to respond well to PARP inhibitors, whereas immunotherapy might be a better option. The team think that both the BRAF and NRAS mutations may cause changes in cell size by affecting levels of a protein known as CCND1, which is involved in cell division, growth and maintenance of the cytoskeleton, as well as its interactions with other proteins.
Commenting on the study, lead author, Professor Chris Bakal, from the Institute of Cancer research, said ‘Cancer cells can shrink or grow to enhance their ability to repair or contain DNA damage, and that in turn can make them resistant to certain treatments.’ He added that the study had a potential diagnostic value. For instance, ‘by looking at cell size, pathologists could predict whether a drug will work, or if the cells will be resistant. In the future, it might even be possible to use AI to help guide the pathologist, by making a rapid assessment about the size of cells and so the treatments that are most likely to work.’