A consultation on the provision of ‘virtual wards’ or ‘hospital at home’ for patients with an acute respiratory infection is being undertaken by the UK’s National Institute for Health and Care Excellence (NICE).
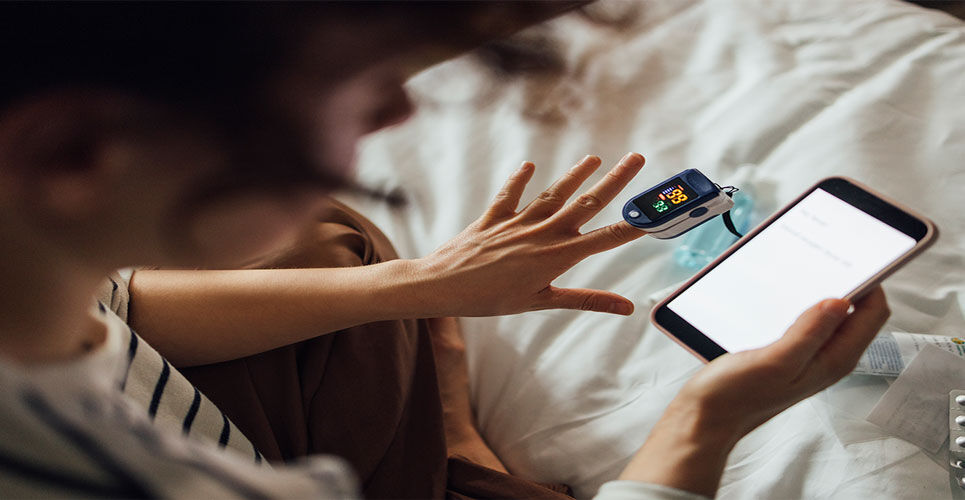
A virtual ward platform technology comprises three key components: a patient-facing app or website, an associated wearable medical devices and a digital platform for healthcare professionals.
NICE has been asked to provide guidance on virtual ward technologies for treating acute respiratory infections because a significant proportion of people needing urgent care from their GPs or in hospital are due to these illnesses.
In its draft guidance, NICE suggests that these wards could be used by those referred for hospital admission, or where someone has been admitted to hospital and their condition is stable or improving but needs ongoing monitoring.
The key operating parameters for effective operation of such a service have also been defined. For example, the virtual ward platform technology should enable interoperability with electronic patient record systems and associated medical devices and devices measuring oxygen saturation should be validated in people with skin of colour.
A further important consideration is the ability to have risk-stratified red, amber or green alerts for healthcare professionals for when readings go outside of the agreed range.

NICE is also keen to ensure that evidence should be generated on a number of key clinical and
cost outcomes including the length of virtual ward or hospital stay and rates of hospital readmission, together with both patient/carer and the healthcare professionals‘ views on acceptability.
Commenting on the use of virtual wards, Mark Chapman, interim director of medical technology and digital evaluation at NICE, said: ‘The NHS is under pressure and giving people with an acute respiratory infection the chance to be monitored from the safety of their own home or care home can help manage capacity in hospitals.
‘Evidence shows virtual wards are safe and can be an option for those who are comfortable using technology to have their condition monitored away from a hospital ward.
‘Using these innovative new technology platforms within a carefully managed NHS environment will enable us to generate the evidence to understand the benefits to patients and the wider health system of using virtual wards.‘
Health minister Helen Whately added: ‘Virtual wards are already allowing thousands of patients to recover in the comfort of their own homes. Expanding them to support people with acute respiratory infections will give more patients the option of recovering at home. At the same time this frees up beds for people who need to be in hospital.‘
‘This draft guidance shows that patients can be monitored at home as if they were being treated in hospital. As part of our Urgent and Emergency Care Recovery Plan the NHS will create an extra 10,000 virtual ward beds by winter, alongside 5,000 hospital beds’.
Evidence presented to the independent committee showed there were similar outcomes for those who were treated in hospital compared with those on a virtual ward. Other evidence showed that people admitted to virtual wards were comfortable using the technology, after training given by a healthcare professional.