Urinary incontinence (UI) is a common, chronic condition which requires long-term management and is associated with significant negative impact on an individual.
Medical management associated with conservative measures still plays an important role in its management. Surgery is still the mainstay treatment of stress urinary incontinence (SUI) but it is not free from complications.
When drugs are prescribed, long-term adherence to therapy is poor. Efforts to improve the clinical effectiveness of pharmacological therapies have included extended release formulations and alternative delivery mechanisms.
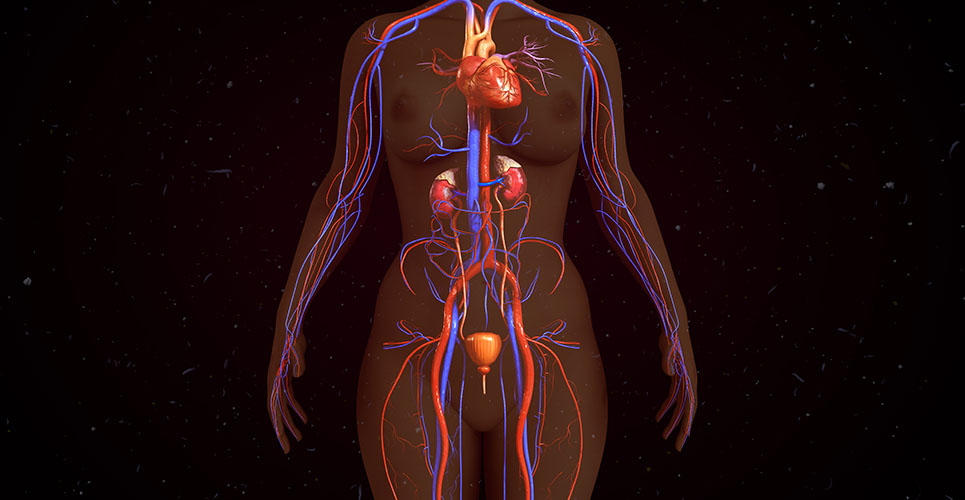
Malfunction occurring at various levels may result in bladder control disorders, which can be classified as disturbances of filling/storage or voiding/emptying. Failure to store urine may lead to various forms of incontinence (mainly urge and stress incontinence), and failure to empty can lead to urinary retention, which may result in overflow incontinence.
The disturbed function can be improved by agents decreasing detrusor activity, increasing bladder capacity and/or increasing outlet resistance.1 Several promising drug targets have been identified to improve the pharmacological treatment of UI.2
In order to instigate appropriate treatment it is mandatory to determine which type of incontinence a patient has and its effect on quality of life. This should be achieved by thorough assessment of UI. This includes a full medical history (including obstetric, gynaecological, surgical, and neurological and medication history), abdominal and vaginal examination, rectal examination (if indicated), completion of a three-day bladder diary, urine analysis and post void residual. If indicated urodynamics and/or imaging should be performed to assess the bladder function and to guide the management.
Drugs for overactive bladder
- Anti-muscarinics
Anticholinergic drugs (also known as antimuscarinics) are the most widely used medication for overactive bladder (OAB). They inhibit the binding of acetylcholine at muscarinic receptors M2 and M3 on detrusor smooth muscle cells and other structures within the bladder wall, thus reducing the contractions of the detrusor muscle and controlling involuntary detrusor contractions without disturbing normal voiding.
- Tolterodine
Tolterodine is a tertiary amine, rapidly absorbed and extensively metabolised by the cytochrome P450 system. It shows no specificity for receptor subtypes but does appear to have relative functional selectivity for bladder over salivary glands.3 The drug is metabolised in the liver to an active metabolite 5-hydroxymethyl derivative and is thought to contribute significantly to the therapeutic effect. Tolterodine is available as immediate release (IR; twice-daily dosing) and extended release (ER; once daily dosing.) The ER form has more advantages over IR in terms of both efficacy and tolerability.4
- Solifenacin
Solifenacin is a tertiary amine and is well absorbed from the gastrointestinal tract (bioavailability 90%). It is a potent M3 receptor antagonist that has selectivity for the M3 receptors over M2 receptors and has much higher potency against M3 receptors in smooth muscle than it does against M3 receptors in salivary glands. It is available in 5mg and 10mg once-daily dosage.
- Darifenacin
Darifenacin is a tertiary amine with moderate lipophilicity and is a highly selective M3 receptor antagonist which has been found to have a five-fold higher affinity for the human M3 receptor relative to the M1 receptor. It has been developed as a controlled release formulation, which allows once-daily dosing. The recommended dosages are 7.5mg and 15mg per day. Trials have shown that it does not cause impairment of memory or other cognitive functions and therefore is particularly good for vulnerable populations such as the elderly and central nervous system (CNS) compromised neurogenic bladder patients.5
- Fesoteredine
Fesoteredine is a new and novel derivative of 3, 3-diphenylpropyl-amine. It is metabolised actively by non-specific esterases to its active metabolite, 5-hydoxymethyltolterodine (5-HMT) which is a potent antimuscarinic agent and is available in 4mg and 8mg once-daily dose.
- Trospium chloride
Trospium chloride is a quaternary ammonium compound which is non-selective for muscarinic receptor subtypes, and shows low biological availability.6 It crosses the blood–brain barrier to a limited extent and hence has few cognitive effects.7 Trospium is available in 20mg twice-daily dosage and as an extended release formulation for once-daily dosing (60mg).
Drugs with mixed action
- Oxybutynin
Oxybutynin is a tertiary amine that undergoes extensive first-pass metabolism to an active metabolite, N-desmethyl oxybutynin, which occurs in high concentrations and is thought to be responsible for a significant part of the action of the parent drug.8 It has a mixed action consisting of both an antimuscarinic and a direct muscle relaxant effect in addition to local anaesthetic properties. Oxybutynin is effective for the management of patients with detrusor overactivity (DO) but the antimuscarinic adverse effects of oxybutynin are well documented and are often dose limiting.9 This is available in the form of tablets, patches, for intravesical application and gel. Gel is the latest preparation which has reduced risks of dermatitis compared to patches but is currently only available in the USA.
- Propiverine hydrochloride
Propiverine has calcium modulating (inhibition of calcium influx causing musculotrophic spasmolysis) and anticholinergic properties. Propiverine is available in an immediate release (15mg TDS) and an extended release preparation (30mg OD). There are efficacy data regarding reduction of frequency of micturition. Recently, the effect of 20mg OD daily has been evaluated showing its efficacy on OAB by improving urgency.10
Anti-depressant
- Imipramine
Imipramine has been shown to have systemic anticholinergic effects: it blocks the re-uptake of serotonin and also has some β agonist activity.11 Some studies have found a significant effect in the treatment of patients with DO12 although others report little effect.13 In light of this evidence and the serious adverse effects associated with tricyclic anti-depressants their role in DO remains uncertain although they are often useful in patients complaining of nocturnal enuresis or bladder pain, and in countries where the more modern and more expensive agents are not available.
- α-adrenoceptor antagonist
The adrenergic receptors found at the bladder neck are α1 adrenergic receptors. Anecdotal evidence has demonstrated that Tamsulosin, a selective α1 adrenoreceptor antagonist, may improve urinary symptoms secondary to detrusor overactivity in men but the results from a randomised, double-blind placebo controlled study would suggest that α adrenoreceptor antagonists alone are not clinically useful in the management of OAB in women.
Intravesical therapy
- Botulinum toxin
This is a neurotoxin which interferes with neural transmission by blocking the calcium- dependent release of the neurotransmitter, acetylcholine, causing the affected muscle to become weak and atrophic. The side effects include bladder pain,14 urinary retention requiring self- catheterisation (20–30%)15 and, rarely, transient muscle weakness.
The main problem is dose-related side effects and there is no clear evidence for the optimal dose of Botox and about the safety of the number of repeated injections patients can have in the treatment of idiopathic detrusor overactivity (IDO).
The dose of Botox can vary from 100IU to 300IU. Higher doses are required for the treatment of neurogenic detrusor overactivity (NDO) while lower doses are advised for IDO. At present the evidence would suggest that intravesical administration of botulinum toxin may offer an alternative to surgery in those women with intractable DO but it is not currently licensed in the UK.
There are two types of Botulinum toxin A available: Botox and Dysport. Most of the studies are done on Botox. Compared to Botox, Dysport is required in higher doses i.e. 500, 750 and 1,000u for the same efficacy.
Hormones
- Oestrogen
Although oestrogen has an important physiological effect on the lower urinary tract, current evidence does not support the use of systemic oestrogens in the treatment of UI as demonstrated by the Women’s Health Initiative (WHI) study.16 However, there is some evidence to suggest a beneficial role for topical vaginal oestrogen in OAB.17
- Desmopressin
Desmopressin (1-desamino-8-D-arginine vasopressin) is a synthetic form of the naturally occurring hormone vasopressin. It has a strong anti-diuretic effect without altering blood pressure. It is a well established treatment for nocturnal enuresis and nocturia, however it has been suggested as a designer drug for daytime incontinence and OAB.18, 19 Desmopressin is safe for long-term use but should be used with care in the elderly due to the risk of hyponatraemia.
Drugs acting on membrane channels
At present there is insufficient evidence to suggest that calcium channel blocking agents and potassium channel opening agents are effective in the treatment of DO.
New preparations
- Vitamin D3 receptor antagonist
The vitamin-D analogues, BXL-628 (elocalcitol) has been shown to have an inhibitory effect on the RhoA/Rho kinase pathway. Up regulation of this pathway has been associated with bladder changes associated with diabetes, outflow obstruction and DO. It remains to be established if the drug will be a useful alternative for the treatment of OAB.
- β3 adrenoreceptor agonist
Beta adrenoreceptor (AR) agonists can inhibit detrusor contractions. There are three types of β- AR found in the human urothelium20 but in both detrusor and urothelium there is a predominance of β3 M-RNA. They induce bladder relaxation by activation of adenylyl cyclase with subsequent formation of c-AMP. YM178 (Mirabegron) in patients with OAB with Tolterodine and placebo as controls has recently been performed. There was a significant reduction in mean frequent micturition frequency (compared to placebo), number of incontinence episodes and urgency episodes per 24 hours. The drug was well tolerated and the most commonly reported side effects were headache and gastrointestinal side effects.21 Phase III studies, just completed, confirm its efficacy and safety profile (Clinical trials.Gov web page,24/4/09, NCT00689104).
Centrally acting drugs
- NK1-receptor antagonist
The main endogenous tachykinins, substance P (SP), neurokinin A (NKA) and neurokinin B, and their receptors, NK1, NK2 and NK3, respectively, have been demonstrated in various CNS regions, including those involved in micturition control. NK1 receptor-expressing neurons in the dorsal horn of the spinal cord may play an important role in DO.
Aprepitant, an NK1 receptor antagonist used for the treatment of chemotherapy-induced nausea and vomiting, significantly improved symptoms of OAB in postmenopausal women with a history of UUI or mixed incontinence (with predominantly UUI), as shown in a well designed pilot randomised controlled trial.22
- Gabapentin
Gabapentin is one of the new first generation anti-epileptic drugs that expanded its use into a broad range of neurological and psychiatric disorders.23 The mechanism of action remains controversial but it has been postulated that it acts by binding to a subunit of α2delta unit of voltage-dependent calcium channels. It needs to be further explored to be proven as a new therapeutic alternative.
- Tramadol
Tramadol is a well-known analgesic drug. It is a weak µ-receptor agonist as well as inhibit serotonin and nor-adrenaline reuptake. Both µ-receptor agonism and amine reuptake inhibition may be useful principles for the treatment of OAB/DO, as shown in a placebo controlled study with duloxetine.24 This needs further evaluation because of its side effects.
- Gonadotrophin releasing harmone antagonist
The effect of this has been demonstrated in the treatment of male lower urinary tract symptoms.25 None of the studies has proven any beneficial effect in females.
Combination therapy
In a highly selected group of patients with neurogenic bladder dysfunction and poor bladder compliance, combination medical therapy with two or three drugs i.e. a combination of anti-muscarinics and Imipramine and/or an alpha blocker, improves compliance and clinical outcomes.26 However, combination therapy requires further study of efficacy and side effects.
Management of stress urinary incontinence
SUI is a common condition in women and is defined as the involuntary leakage of urine during increased abdominal pressure in the absence of a detrusor contraction. It can be either due to hypermobility of the urethra due to weakness of the pelvic floor support and/or intrinsic sphincter deficiency.
The pharmacological treatment of SUI aims to improve the intraurethral closure forces by increasing the tone in urethral smooth and striated muscle. Several drugs contribute to such an increase,27 but relative lack of efficacy or/and side effects have limited their clinical use. Drug therapy is usually reserved for women unfit for surgery, women awaiting surgery, women who have yet to complete their families and for those women who do not want surgery.
- Duloxetine
Duloxetine is a combined serotonin and noradrenaline reuptake inhibitor, which has been shown to increase urethral sphincter muscle activity during the storage and filling phase of micturition.28 Duloxetine is lipophilic, well absorbed and extensively metabolised. Hashim and Abrams have suggested that the drug should be started at a low dose of 20mg twice-daily for 2 weeks which can then be increased to the recommended dose of 40mg twice-daily to reduce nausea.29 Nausea was the most common adverse event but other side effects include vomiting, constipation, dry mouth, dizziness and insomnia. It is licensed for the treatment of SUI for women with moderate and severe incontinence in Europe.
Management of nocturnal enuresis
For many women with nocturnal enuresis (NE), investigations will reveal a picture of detrusor overactivity. It is important to review a completed frequency volume chart to rule out nocturnal polyuria and in some cases referral to other specialities may prove helpful in management as certain conditions can be linked e.g. sleep studies to assess for sleep apnoea. Medications used in the treatment of OAB may prove beneficial in the treatment of NE. However, there are other drugs used more specifically for NE. Desmopressin, a synthetic vasopressin analogue has a potent anti-diuretic effect and is used in the management of diabetes insipidus and NE.
Tricyclic antidepressants may also be used in the management of NE. Amitriptyline has been shown to be effective in reducing the number of enuresis episodes. Imipramine has been shown to have systemic anticholinergic effects. However, these drugs should be used with caution in the elderly due to cardiac side effects and the increased risk of falls.
Management of overflow incontinence
Incomplete bladder emptying as a result of voiding dysfunction can lead to overflow incontinence. The main aim in the management of voiding dysfunction is to improve urinary flow and ensure complete bladder emptying. Voiding dysfunction can be the result of a urethral stricture, detrusor sphincter dysynergia or an underactive bladder. Women with persistent urinary residuals are also at risk of developing recurrent urinary tract infections which may also cause urinary leakage.
Parasympathomimetics stimulate contraction of the detrusor muscle.30 Examples of these include distigmine bromide and bethanechol chloride. However, if the patient also has UUI this can worsen their symptoms. Alpha antagonists cause relaxation of the striated muscle of the urethral sphincter. Examples of these include alfuzosin, doxazosin, prazosin and tamsulosin.
Conclusion
There are various drugs available on the market to help in the management of UI but anti-cholinergics still remain the first line of treatment for OAB. Compliance and persistence is poor because of side effects. New drugs are under development. Accepted drug treatment for SUI is scarce. Duloxetine is the only licensed drug available. New targets for control of micturition are being defined, but further research is needed to advance the pharmacological treatment of micturition disorder.
Authors
Monika Vij
Walsgrave University Hospital of Coventry, UK
Vijay Anand
York House Medical Centre, UK
References
1 Wein AJ. Pathophysiology and categorisation of voiding dysfunction. In Walsh P, Retik A, Wein AJ (eds): Campbells Urology, Eighth Edition. Philadelphia: Saunders; 2002, 887-98.
2 Andersson KE. Neurourol Urodyn 2007;26
(Suppl. 6):934-47.
3 Nilvebrant L et al. Eur J Pharmacol 1997b;
327:195-207.
4 Van Kerrebroeck et al. Urology 2001;57(3):414-6.
5 Kay GG and Ebinger U. Int J Clin Pract 2008;62, 11:1792-1800.
6 Schladitz-Keil G et al. Arzneimittel Forsch/Drug Res 1986;36:984-7.
7 Fusgen I and Hauri D. Int J Clin Pharmacol Ther 2000;38(5):223-34
8 Hughes KM et al. Xenobiotica 1992;22:859-69.
9 Baigrie RJ et al. Br J Urol 1988;62:319-22.
10 Lee KS et al. BJU Int vol 105 1565-1570, June 2010.
11 Baldessarini KJ. Drugs in the treatment of psychiatric disorders. In: Gilman et al. (eds.) The pharmacological basis of therapeutics, 7th edition. New York: McMillan Publishing Co; 1985. 387-445.
12 Castleden CM et al. Age Aging 1986;15:299-303.
13 Diokno AC et al. J Urol 1972;107:42-3.
14 Karsenty G et al. Eur Urol 2008;53(2):275-87.
15 Sahai A et al. J Urol 2007;177(6):2231-6.
16 Hendrix SL et al. JAMA 2005;293(8):935-48.
17 Cardozo L et al. Acta Obstetr Gynaecol Scand 2004; 83:892-7.
18 Robinson D et al. BJU Int 2004;93:996-1000.
19 Hashim H et al. Neuro Urol 2009:28:40-6.
20 Otsuka A et al. Naunyn Schemiedebergs Arch Pharmacol 2008;377:473-81.
21 Chapple CR et al. Eur Urol Suppl 2008;7(3):239 (abstract 674).
22 Green SA et al. J Urol 2006;176(6 Pt 1):2535-40.
23 Striano P and Striano S. Drugs Today (Barc) 2008;44(5):353-68.
24 Steers WD et al. BJU Int 2007;100:337-45.
25 Debrutne F et al. Eur Urol 2008;54(1):170-7.
26 Natalin R et al. World J Urol (2010) 28:79-85
27 Andersson KE. Drugs 1988;35:477-94.
28 Katofiasc MA et al. Life Sci 2002;71(11):1227-36.
29 Hashim H and Abrams P. Drugs 2006;66(5):
591-606.
30 Henry J (Ed). The British Medical Association New Guide to Medicines and Drugs. London: Dorling Kindersley; 1998.