teaser
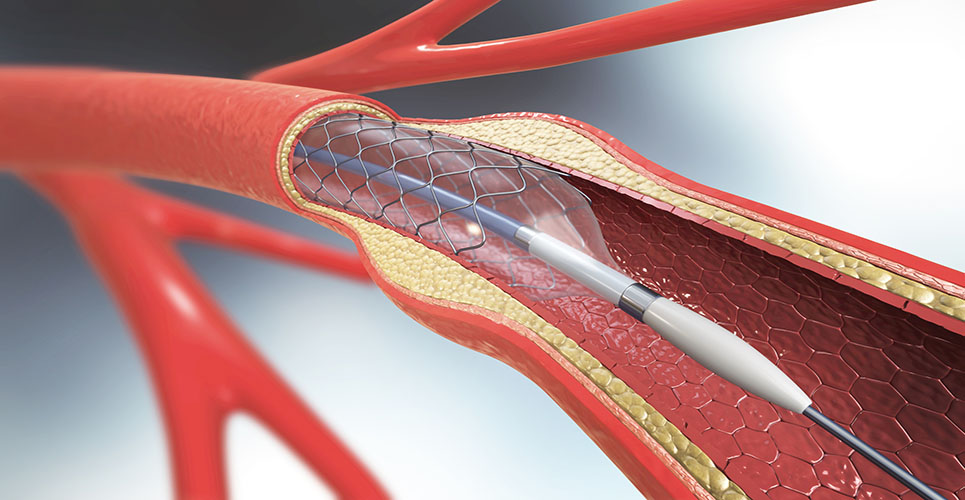
Preliminary study findings have shown higher long-term mortality with a drug-eluting than a bare-metal stent in setting saphenous vein graft (SVG) coronary artery lesions.
However, further studies are needed before firm conclusions can be drawn regarding the safety of using drug-eluting stents (DESs) for SVG lesions, write Dr Pierfrancesco Agostoni, of Antwerp Cardiovascular Institute, Belgium, and co-authors in the Journal of the American College of Cardiology.
SVG lesions represent between 10 and 15% of all lesions on which percutaneous coronary interventions (PCIs) are performed, Agostoni et al. note. Yet lesions in SVGs have been all but completely excluded from pivotal trials of DESs, they say.
In light of this, and the ongoing debate surrounding the safety of DESs, the researchers conducted a long-term follow-up analysis of the RRISC (Reduction of Restenosis in SVGs with Cypher) trial.
The original findings of the RRISC trial were that sirolimus-eluting stents (SES) resulted in fewer six-month angiographic and clinical indicators of restenosis than BMS in SVG lesions.
The study included 75 patients with a history of coronary artery bypass surgery and with 96 “de novo” target lesions localised in 80 diseased SVGs. Patients were randomly assigned to receive SESs or BMSs, with 38 patients receiving 60 SESs for 47 lesions and 37 patients receiving 54 BMSs for 49 lesions.
Over a median follow-up period of 32 months, 11 (29%) patients in the SES group died compared with none in the BMS group (p<0.001).
Number-needed-to-harm analysis showed that treatment of 3.4 patients with SESs resulted in one additional death compared with BMS treatment.
The authors note that seven of the 11 deaths had cardiac causes. Three were sudden, possibly related to late or very late stent thrombosis, and one was caused by angiographically documented very late stent thrombosis 13 months after implantation, which caused myocardial infarction leading to death.
The team also found a nonsignificant trend toward an increased rate of target-lesion and target-vessel-related revascularisation procedures in the SES group beyond six months, neutralising the initial six-month benefit of SES.
The authors conclude: “The use of BMS was associated with lower long-term mortality than the use of SES for SVG disease. Also, the six-month reduction in repeated revascularisation procedures shown with the use of SES was lost at longer-term follow-up.”
Nevertheless, they add: “Because the observations seen in this secondary post-hoc analysis may have arisen from the play of chance or other clinical factors unrelated to stent type, further studies are required before conclusions can be made about the safety or harm of using SES for SVG lesions.”
J Am Coll Cardiol 2007;61:689-94